Learn All About Pelvic Organ Prolapse and the Role of Yoga in Recovery
Yoga can help manage pelvic organ prolapse, but there are also some poses, movements and breathing methods that could make the condition worse.


Many women are told at their 6 week postpartum follow-up, that they are cleared for sexual intercourse, however, most women do not return to sexual intercourse at this time frame, for several reasons1,2. If this is you, you are not alone, and you are actually in the vast majority. During this unique time in a woman’s life, she is experiencing physical, emotional, and relational changes that all influence a woman’s sexuality. Physically, many women experience pain with sex, lack of desire, and decreased lubrication2.
One of the biggest causes found to contribute to these symptoms was hormonal changes related to whether a woman is breastfeeding during the postpartum period or not. While breastfeeding can offer a host of benefits, for mom and baby, it can be a cause of pain with sex because of the decreased sex hormones impacting the tissue of the vagina and vulva2,3, leading to a condition called vulvodynia. For more information about this condition, and if this sounds like you, check out this blog post to learn more.

Do you feel a bulge or feel like you are sitting on a ball in the pelvic area? What should you do? Don’t freak out, there is help for you! Here are some things to get you started:
Not all prolapses are the same. They can vary based on which organ is descending and how far it has descended (grade).
Prolapse will be diagnosed based on which organ is descending:

Medically, the answer is a resounding ‘no’… but postpartum sex is still an understandable concern for most pregnant women, especially in a digital age where whispered rumors have given way to detailed stories of difficult birth experiences splashed across social media pages.
In the greater debate over vaginal birth vs. C-section, the real issue on the minds of many expectant mothers is often whether one mode of delivery is somehow better than the other. It’s a complex question; but a group of researchers in Ontario, Canada recently attempted to answer the ‘sex after baby’ part of it. What they found out surprised even them; and shed some important light on the bigger question as well.

From bullet journals to hot yoga, and five minute breathing exercises to weekend meditation retreats, mindfulness is the hashtag-goals wellness buzzword of the moment… and rightly so. It’s hard to argue with all the documented health benefits of being fully present in your activities and relationships.
But is mindfulness a magic cure for painful sex? That’s what many of my patients have been told by well-meaning friends, partners, and even medical practitioners and professional counselors. And I’ll tell you what I tell them:
The pain isn’t in your head; it’s in your muscles. It’s in your nervous system. It’s a complex interplay of the two in many cases.

Luckily there are many wonderful treatments that can stop the cancer, either completely or from progressing further. However, the treatments do come with some unwanted side effects. But there is help and having a pelvic floor physical therapist added to your ervical cancer support team can truly guide you along the way.
Some common treatments are pelvic external beam radiotherapy and/or brachytherapy, which unfortunately can adversely affect women’s sexual functioning and quality of life. Radiotherapy especially can cause vaginal stenosis, which is narrowing of the vaginal canal. This is due to radiation effects of collagen deposition, loss of elasticity in the vaginal tissue, and atrophic changes of the mucosa. Unfortunately, 88% of women after radiation will develop vaginal stenosis. As you can imagine, narrowing of the vaginal canal can impede women’s ability to tolerate penetrative sexual intercourse or gynecologic exams, for example.

January is a great time to make resolutions, fresh starts, and to start committing to self-care! It is also Cervical Health Awareness Month. Today we chat about the Pap test. If you are an adult with female anatomy living in the United States, chances are you have heard the term “Pap test” or “Pap smear.” But why they are important and what can you do if you can’t tolerate a gynecological exam with a speculum?
Pelvic floor issues such as vaginismus, vulvodynia, and vulvar vestibulitis can make it hard to have anything inserted into the vagina. Be it a penis, tampon, or a speculum, commonly reported symptoms include intense burning and stinging, sharp pain, a feeling that you “will tear,” or like you are “hitting a wall.” These are all conditions that are treatable atFemina Physical Therapy. Our therapy along with your healthcare team can help restore your ability to take care of your reproductive health as well as your sexual health and pleasure.

Personal lubricant (lube) is something most people will use at least once during their sexual lifetimes, if not every time they are sexually active.
Lubricants are fluid or gel substances designed to offset genital dryness or inadequate natural lubrication which can be associated with discomfort or pain with sex or general activity. Lubes can be used for sexual activity, or just to alleviate dryness throughout the day.
A lot of our references for intimacy come from what we see in our families, movies, and for sex, a lot of the time porn. What we are individually exposed to will possibly become what we think is the norm, which can then possibly skew our views towards intimacy with a partner. For instance, if a woman watches porn for a sex reference she may think her vulva has to look a certain way or that she needs to attain an orgasm with penetration or to be intimate with her partner she has to have sex, when that’s not really the case.

If you are thinking “YES,” you are not alone. In a study by Bahouq et al. in 2013, 81% of clients with low back pain reported sexual problems and 66% of those clients reported never bringing the subject up with their doctor. As we all know, sex is an important activity for many. Today’s post will shine a light on the latest science based recommendations sex positions for those with low back pain and how the therapists at Femina PT can help.

I came across an article that came out last month and it brought up an old question I often muse over--Does Vaginismus create the fear and anxiety in women, or does an underlying fear or anxiety create Vaginismus? As we often say in physical therapy "It depends".
With some of my patients, there is a specific injury or infection that is at the root of their pain. The story is similar whether they were diagnosed with Vaginismus, Vulvodynia, Vestibulitis, Dyspareunia, or a host of many other diagnoses that lead to painful intercourse. For example, a young girl that always wore bathing suits and developed recurrent yeast infections, only to find out that over a decade later she had developed vaginismus. She had no fear or anxiety going in to first sexual encounter, yet she had severe pain. Now, she presents with what I perceive as fear and anxiety. Should she be treated for fear and anxiety? Or just the pain? Or both?

Eating disorders are unfortunately common, with at least 9% of people worldwide suffering from an eating disorder. This translates to 28.8 million Americans will have an eating disorder in their lifetime. There are different types of eating disorders (ED) including anorexia nervosa, bulimia nervosa, and binge eating disorder. Other than the typical psychological and social implications that these eating disorders may cause, they also can affect our pelvic health and lead to pelvic floor dysfunction. It can lead to incontinence (either urine or feces), prolapse, increased urinary urge, pelvic pain (possibly associated with polycystic ovarian syndrome or PCOS), constipation, and sexual dysfunction.

Pain, fatigue, and other symptoms associated with endometriosis can affect quality of life, including sexual health and happiness. In fact, a study published last year found that patients with endometriosis have more than twice the sexual dysfunction as compared to women without the disease (Fairbanks, Abdo, Baracat & Podgaec, 2017). Below is a list of common sexual health problems associated with endo and some strategies to help:
Some people with endometriosis report that pain and fatigue can be better or worse at certain times of the month. Keeping a diary can help identify patterns of pain associated with the cycle. Estrogen levels peak during ovulation, usually day 12-15 of the cycle, leading to higher pain levels for some with endometriosis. Knowing how your body feels during different parts of the cycle can help you make decisions about when to engage or avoid in sex to manage your pain.

Endometriosis is a global disease affecting 5-15% of women during their reproductive years. It is characterized by the presence of endometrial-like tissue outside of the uterus which can trigger a local inflammatory response and can have a significant impact on patients’ quality of life.
One such domain of quality of life that is often affected is the correlation between endometriosis and sexual function. The DSM-V defines sexual dysfunction as a clinically significant disturbance in a person’s ability to respond sexually or to experience pleasure and includes pelvic pain, penetration disorders, lack of sexual interest, and/or arousal and orgasm disorders. Unfortunately, it is common, as approximately 40% of women with endometriosis and chronic pelvic pain suffer from sexual dysfunction.

Foam rolling is a fantastic way to manage pelvic pain by keeping your tissues hydrated with increased blood flow, reducing trigger points in the muscles and fascia, and improving mobility and range of motion. Foam rolling has also been found to increase parasympathetic nervous system response (rest and digest) which is also helpful in chronic pain management (Beardsley, 2015).
I often tell my patients that the pelvic is not an isolated island, in fact it’s at the center of your body and deeply intertwined with many body functions including balance, movement, toileting, and sex. Go ahead and palpate your pelvic bones- you can feel that the muscles to the back, hip, and legs all attach to the pelvis. When there is dysfunction in these muscle groups, pelvic pain, pelvic mal-alignment, and tight pelvic floor muscles can be a result. By keeping these tissues healthy and mobile can help manage your pelvic pain.
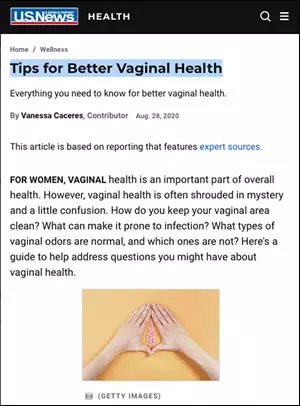
Here is an excerpt from this thorough and very informative article by Vanessa Caceres:
For women, vaginal health is an important part of overall health. However, vaginal health is often shrouded in mystery and a little confusion. How do you keep your vaginal area clean? What can make it prone to infection? What types of vaginal odors are normal, and which ones are not? Here's a guide to help address questions you might have about vaginal health.

Chronic psychosocial stress is defined as either a major life event that takes place over a long period of time (ie. death of a family member) or small stressors that are constant and often accumulate (ie. traffic, financial worries, work deadlines).1,2 A study by Allen Kanner, Ph.D, published in the National Library of Medicine, found that these small stressors can have more of a negative effect on health than the more severe but less common stressors.1

Many factors come into play when considering resuming to sexual activity postpartum. Individuals who have just given birth are not only faced with potentially new physical aches and pains, but also shifting family and partner dynamics, which all play a role in painful sex and lowered sexual desire.
One study reported both of these common postpartum conditions as prevalent as 22% experiencing painful sex and 86% experiencing loss of desire2. It is common in postpartum rehabilitation to be prescribed specific pelvic floor exercises in order to help strengthen the pelvic floor.

Here are some ways you can involve your partner in your pelvic floor physical therapy:
Both studies and clinical experience have shown that talking to your partner about your sexuality, pelvic floor issues, and sharing the progress you’re making in pelvic floor therapy can improve anxiety, reduce pain levels, and bring more intimacy to your relationship. As you transition to sex with your partner, sexual assertiveness will also help you find activities, angles, and positions that feel pleasurable, not painful to you and your partner.

There are many health benefits to cycling, including improved cardiovascular health, better weight control, and decreased risk of breast cancer in women (Greenberg, 2019).
Despite all these amazing health benefits (I, myself am an avid bicyclist), you can ask almost anyone who has ridden a bike- the seats can get kind of uncomfortable after prolonged periods of time. And for some, issues worse than discomfort can arise: genital numbness, genital pain, nerve conduction issues, and sexual dysfunction. Through the years there has been some research that has linked bicycle riding, genital pain and genital numbness, and sexual dysfunction in both sexes. In fact, we’ve explored how rider/seat positioning on your bicycle can exacerbate nerve and orthopedic issues in past blogs.

Risks and Possible Benefits
In the past decade, nonsurgical devices using radio-frequencies, lasers, and infrared light have been marketed as non-invasive treatments for “vaginal rejuvenation.” However, there has been conflicting opinion among the medical community as to what the lasers have evidence of treating. The rampant use of the lasers to treat conditions they have not been approved to treat has also caused the Food and Drug Administration to warn the public about these devices in 2018.

This article will review the research related to these, but in reading, know that we believe your pain is real and should be addressed from all relevant contributing factors.
A very large range, about 7-46% of Americans may experience painful sex. For some, it may be a one-time painful experience, and for others, it may be every single time. This can have a huge effect on mental health and overall quality of life.
Studies have shown that mindfulness can improve your sex life by increasing arousal, reducing sexual pain, lowering judgement, improving relationship satisfaction, and improving self esteem. Those of you who have had sessions with me in the clinic have most definitely practiced some forms of mindfulneses meditation with me, as it helps one increase connection between the brain and body, reduce anxiety, and downregulate the nervous system.
Mindfulness can be defined as an open or a receptive attention to and awareness of what is taking place, both internally and externally, in the present moment (Barnes et al., 2007).
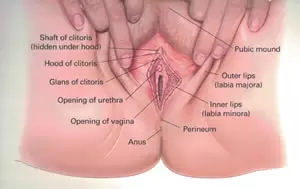
One of the most empowering things you can do for your pelvic health is to take a look at yourself in the mirror and learn your anatomy. Here is a quick primer on how to stay on top of what's going on down there, including tips on simple self examination and resources to find more information.

The medical community recently had a major a-ha moment about painful sex. It’s something the women who suffer from it have always known – but the results of a recent study about it could be a game-changer for treatment.
Whether you have a clinical diagnosis like vaginismus or dyspareunia, or you just know that sex hurts, painful sex is a common problem - almost half of all women will experience it at some point in life. More than 20% of premenopausal women say sex is painful; the prevalence is higher in women under 30. For some, it’s difficulty during intercourse; for others, it’s significant pain upon penetration. Still, others may not be able to experience penetration at all.

Our team at Femina Physical Therapy is committed to providing the highest level of evidence-based care. That is why we are conducting a research study to determine the effectiveness of low intensity shockwave therapy for painful intercourse, or dyspareunia as it is known clinically. We are searching for volunteers to participate in this high quality study. Those who qualify to participate will receive a significantly reduced rate on all visits related to the study + will receive our world-class physical therapy program for treating painful sex!

Yoga can help manage pelvic organ prolapse, but there are also some poses, movements and breathing methods that could make the condition worse.
"Prolapse" refers to a descending or drooping of organs. Pelvic organ prolapse (POP) refers to the prolapse or drooping of any of the pelvic floor organs, including: the bladder, uterus, vagina, small bowel, or rectum. These organs are said to prolapse if they descend into or outside of the vaginal canal or anus.
Read our previous blog for more information on prolapse and how pelvic floor therapy can help.
Yoga has been found to help women with urinary incontinence, but will it help with prolapse?

The diagnosis itself is not well known among healthcare practitioners yet alone the general public. Those who experience its symptoms can be hesitant to talk about it with their healthcare practitioners even though it may be affecting their quality of life.

Endometriosis is a global disease affecting 5-15% of women during their reproductive years. It is characterized by the presence of endometrial-like tissue outside of the uterus which can trigger a local inflammatory response and can have a significant impact on patients’ quality of life.
One such domain of quality of life that is often affected is sexual function. The DSM-V1 defines sexual dysfunction as a clinically siginifcant disturbance in a person’s ability to respond sexually or to experience pleasure and includes: pelvic pain, penetration disorders, lack of sexual interest and/or arousal and orgasm disorders. Unfortunately, it is common, as approximately 40% of women with endometriosis and chronic pelvic pain suffer from sexual dysfunction.

Many of our patients experience sexual dysfunctionandanxiety, depression and chronic pain. These conditions are known to coexist, and we unpack each component of pain, mood and one’s behaviors, desires and attitudes related to sex and physical intimacy.
Pelvic girdle pain isdefined as “pain between the posterior iliac crests and gluteal folds particularly in the vicinity of the sacroiliac joint” (Simonds). More simply stated: in the very low area of your back and buttock. Pelvic girdle pain is common postpartum and may impact disability in the fourth trimester. Many are aware of peripartum symptoms such as low back pain, incontinence,pelvic organ prolapse, pain with intercourse, and postpartum depression. Knowing that many women experience pain during and after pregnancy - what can we learn about the effects of pelvic girdle pain? Specifically, what impact does pelvic girdle pain have on symptoms of mood and sexuality?

Acording to the American College of Obstetricians and Gynecologists (ACOG), a hysterectomy is surgery to remove the uterus. It is a common type of surgery for women in the United States.

That’s a good thing; intimacy is an important factor in your relationship and your own well-being. But whether this is your first baby, or you’re sure it’s your last, your anticipation might be tinged with some anxiety. After all, your body has been through a lot since that positive pregnancy test result.
Sleepless nights, fluctuating hormones, and breastfeeding challenges can take a toll. Perhaps you’re still healing from a C-section or a physically challenging delivery. Even if giving birth was a breeze, and this is your easiest baby yet, you may worry that your expectations aren’t in sync with your partner’s.
When it comes to your postpartum sex life, what’s the new normal? And how soon can you get there?
Sadly, research shows that’s much more likely to be true for men than it is for women. In fact – although sexual function after bladder removal is ‘routinely considered’ for male patients – surgeons in one study discussed complications that could affect pelvic health and sexual function with just 13% of female patients. Worse, the medical counseling those women got after surgery ignored the topic of sex altogether.
It's no surprise that if you recently had hip surgery - or have an ongoing hip issue - that your sex life could suffer. Read on for some recommendations.
Femoroacetabular impingement (FAI) syndrome is a disorder of the hip that typically affects young adults. It is the result of an abnormal contact between the greater trochanter of the femur (thigh bone) and the acetabulum (the socket).

A 2016 study by McNicoll et al. suggests that Sexual Assertiveness,or the ability to communicate openly to your partner about your sexual experience, may reduce the pain experienced with provoked vestibulodynia (PVD), increase sexual function, and encourage your partner to communicate you in ways that help boost your sexual health.
Pelvic pain and pain with sex may come from several different avenues, including vaginismus, vulvodynia, vestibulodynia, endometriosis, or tissue changes caused by menopause. The 2016 study by McNicoll et al. specifically worked with women with provoked vestibulodynia.

Sexuality can be a big part of who we are as individuals. Sexual function can be defined as “specific physical, physiological, neurological and emotional behaviors expressed by an individual response”.5 Sexual function and cancer can have an important and detrimental relationship. There are certain cancers that can unfortunately affect our sexual health, including cervical, ovarian, bladder, kidney, colorectal and breast cancer to name a few.
Some cancer treatments can cause unwanted side effects that affect our sexual health such as decreased sexual arousal or desire, vaginal stenosis (narrowing of the vaginal canal), dyspareunia (painful sexual intercourse), and bladder/bowel dysfunction. This can affect our relationships with ourselves and with our partners, and reduce quality of life.

Through the last year and half, we have learned more about COVID-19 and each and every day new data helps us better understand this virus and how to practice safe sex during COVID.
The virus spreads through infected saliva, mucus, or respiratory particles entering the eyes, nose, or mouth. This means it can be transmitted through kissing and close contact. Studies have also detected the virus in feces and in sperm in those infected (Diangeng et al., 2020). It is unknown at this point if the virus can be spread through sperm or feces. Educating yourself can be the key to safe sex during COVID-19.

Sexual problems are a side effect of cancer treatment that oncologists don’t often talk about, but there are treatments to help, including the pelvic floor therapy that we do at Femina PT. Surgery, chemotherapy, radiation, hormonal therapy, stem cell transplantations, and other procedures can negatively affect quality of life, including sexual health and happiness. These side effects are not limited to cancers of the sexual organs either. Cancer treatment anywhere in the body (cervix, breast, throat, GI tract) can lead to changes in sexuality.

A 2019 study by Towe et al., found that certain medical issues including metabolic syndrome, obesity, and eating disorders have an effect on female sexuality. The study also found evidence that incorporating of healthy dietary patterns into everyday life may positively influence female sexuality.
According to the Mayo Clinic, Metabolic Syndrome is a “cluster of conditions that increase the risk of heart disease, stroke, and diabetes. Metabolic syndrome includes high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels. The syndrome increases a person's risk for heart attack and stroke.” Those with Metabolic Syndrome often have apple or pear shaped bodies.

The world is learning more and more about the pelvic floor and the many ways that it can be treated. At Femina Physical Therapy, we have spoken about pelvic rehab for urinary, bowel, birth, pregnancy, bladder, erectile issues, and many more. But we all know the question that everyone wants answered: Does pelvic floor strength affect orgasm?
Well reader, you came to the right place.

About 5-10% of reproductive aged persons with female-associated genitalia have endometriosis. Symptoms can range from no symptoms to debilitating pelvic pain with dysmenorrhea, pain with periods, abdominal pain, genital pain, bladder dysfunction, bowel dysfunction and other chronic overlapping pain conditions. In addition, endometriosis is known to also affect sexual quality of life. Pain with sex is called dyspareunia; while deep infiltrating endometriosis is a more severe form of endometriosis.
It’s Pelvic Organ Prolapse Awarenesss Month. Today we talk about something that’s often not talked about and lay out ways prolapse can be avoided and treated with proper pelvic floor physical therapy.
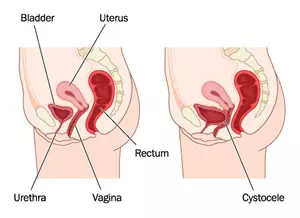
"Prolapse" refers to a descending or drooping of organs. Pelvic Organ Prolapse (POP) refers to the prolapse or drooping of any of the pelvic floor organs, including: the bladder, uterus, vagina, small bowel, or rectum. These organs are said to prolapse if they descend into or outside of the vaginal canal or anus.
Prolapse is sometimes given these specific names to describe which organ is descending:
Cystocele:The bladder falls backward into the front (anterior) vaginal wall
Urethrocele:A prolapse of the urethra (the tube that carries urine) into the vaginal wall
Uterine prolapse:prolapse of the uterus
Vaginal vault prolapse:prolapse of the vagina
Enterocele:Small bowel prolapse
Rectocele:the rectum falls forward into the back (or posterior) vaginal wall.

There are many reasons why those born with female anatomy may require the use of a vulvovaginal moisturizer throughout their lifetime. As you age, the vaginal and vulvar tissues tend to become drier and less elastic. This change is typically seen around the time one goes through menopause due to the drop in estrogen that occurs. The vulvovaginal tissues are very sensitive to hormonal changes and estrogen is the hormone that controls vaginal lubrication, as well as tissue elasticity and thickness.

In addition to giving you insight into what you like sexually, masturbating can help you uncover what you don’t like. It can also help you uncover information about your body.
You can learn so much about your pelvic floor and anatomy through masturbation,” says Dr. Jeffcoat.
For instance, if you learn that vaginal penetration hurts when you masturbate, you will have specific insights on where the hurt is, and you can bring those insights to a licensed pelvic health provider. Similarly, if you discover that you have a difficult time having an orgasm or can't have one at all, "[t]his could be due to a hormonal imbalance or simply weak or uncoordinated pelvic floor muscles,” says Dr. Jeffcoat. The strength and tone of your pelvic floor muscles play a role in determining sexual wellness and satisfaction.

As pelvic floor physical therapists, we work with a lot of women who have some type of female sexual dysfunction, whether it may be pain with initial penetration, pain with deep thrusting/deep penetration, pain with orgasms, or decreased sexual arousal, desire, libido. Unfortunately, about 30-50% of women may suffer from these symptoms.

Many patients with IC have other overlapping pain conditions such as Dyspareunia (pain with intercourse). 88% of patients with IC had at least one symptoms of sexual dysfunction (lack of sexual interest, can’t relax and enjoy sex, difficulty becoming sexually aroused and difficulty reaching orgasm)1. Women with IC rated their sexual dysfunction as moderate to severe when compared to controls and reported increased pain with intercourse, decreased desire and decreased frequency of orgasm5,6.
I was on a recent plane flight and sat next to two women that were very chatty with one another. They quickly swept me up into their conversation. Inevitably, in situations like this, everyone asks “So what do you do for a living?”. My answer used to be “I’m a physical therapist”. The past couple of years, my standard response is “I’m a physical therapist, but let me tell you about what kind of physical therapist I am”. Then I go into the diagnoses I treat related to bowel, bladder and sexual health and, in general, how I treat them. Across the board, their reaction is a mix of astonishment and genuine interest. The follow up dialogue is always eye-opening for them, and more often than not, they will report either knowing someone close to them as having one of these pelvic floor issues, or they have it themselves.

Haga clic aquí para la versión española Sex Without Pain: A Self-Treatment Guide To The Sex Life You Deserve was written by Heather Jeffcoat, DPT, a physical therapist with countless successes in treating pain of this type. Women with vaginismus, overactive pelvic floor, painful intercourse, vulvodynia, vulvar vestibulitis, vestibulodynia, dyspareunia, interstitial cystitis have all benefited from her unique program. Heather uses her orthopedic background to approach treatment of these muscles like they are....muscles! She utilizes a self-treatment tool called a dilator to provide massage and other muscle relaxation and stretching techniques in a gentle fashion to return a women's muscles back to a resting, rather than guarded, state.
• To order "Sex Without Pain" in paperback from Amazon for $24.99, click here.
• To order an electronic read-only non-printable PDF copy of the book for instant download at $19.99, use the button below:
• To schedule an appointment at one of the Femina PT offices, click here.
• For a list of other trusted health care providers, click here.
I went to Heather after the birth of my third child. It was lucky, really, that I was referred to her, because my doctor had referred me to a surgeon for a possible hysterectomy or pelvic wall rebuild. Thankfully, I went to Heather before undergoing either surgery, she was able to fix the problem. She has studied extensively in women's health--even written a book about it--and was able to diagnose my problem, suggest a course of treatment (6 weeks), and then follow...
"I had a severe tear during childbirth that was not stitched together correctly and therefore healed poorly. Even after having a surgery a year later to remove the scar tissue, I was still having pain, and no one could explain why -- there was no overt 'reason' to explain the pain. I had tried other 'specialists' and even saw another physical therapist who had me do hip / leg stretches -- what a joke! I was about to give up and just 'live with it' until thankfully I kept...
A personal journey and testimonial from one of my patients: I was diagnosed with vaginismus 4 years ago. I never heard of such medical condition until after I got married. At first my husband and I didn't know what to do, we didn't know what the issues were or how to overcome it. Being born and raised in Armenia and being Christian I wasn't that open about talking to sex with others and so it wasn't easy to seek help. But eventually I went to an Ob-Gyn and luckily she...

Like what you are seeing so far? Register for our mailing list and receive periodic updates via email, a 15% discount code for the "Sex Without Pain" ebook, and instant access to our Downloads area!