Alphabetical Index of Articles on Women's Sexual, Pelvic Floor, and Reproductive Health
Chronic Constipation | The Basics

Dealing With Chronic Constipation? Read On.
Most people experience constipation from time to time. Constipation isn’t just the inability to have a bowel movement, it includes the difficulty associated with bowel movements. Travel, inactivity, illness, and certain over the counter medications taken “as needed” commonly result in short-term or acute constipation. Constipation lasting longer than three months is considered chronic constipation. Chronic constipation should be treated by a doctor to prevent health complications.
Clear communication is essential to working with doctors, but the general public often has only a rudimentary understanding of medical terms - including constipation. There is often a gap between the physician and the patient’s perception of constipation which can lead to confusion. (1, 2, 7, 10) A study of people who thought they had constipation showed that only a third actually fit the criteria for constipation, while the rest actually had Irritable Bowel Syndrome or other gastrointestinal disorders. (9) So what are the criteria for constipation?
Eating Disorders and Pelvic Floor Dysfunction | ED Awareness Week

What's the Connection Bewteen Eating Disorders and Pelvic Floor Dysfunction?
Read on for some answers.
Eating disorders are unfortunately common, with at least 9% of people worldwide suffering from an eating disorder. This translates to 28.8 million Americans will have an eating disorder in their lifetime. There are different types of eating disorders (ED) including anorexia nervosa, bulimia nervosa, and binge eating disorder. Other than the typical psychological and social implications that these eating disorders may cause, they also can affect our pelvic health and lead to pelvic floor dysfunction. It can lead to incontinence (either urine or feces), prolapse, increased urinary urge, pelvic pain (possibly associated with polycystic ovarian syndrome or PCOS), constipation, and sexual dysfunction.
How Obesity Increases Urinary Incontinence

Learn How Obesity Increases Urinary Incontinence and How Pelvic Floor Therapy Can Help
Urinary Incontinence is common, why suffer?
Urinary incontinence is the loss of bladder control.Urinary incontinence affects up to 1 in 3 women. The two most common types of urinary incontinence that affect women are stress incontinence and urge incontinence (also called overactive bladder, or OAB). Incontinence affects twice as many women as men. This may be because pregnancy, childbirth, and menopause are contributing factors to urinary incontinence. Urinary incontinence should not be considered a normal part of aging, and it can be treated.
A new article published in September, 2018 by Lamerton, Torquati, & Brown found that being overweight (BMI 25-30) increased risk of urinary incontinence for young and middle aged by 35% and obesity (BMI ≥30) almost doubles the risk at 95%.
How to Have Your Best Poop Ever: Solutions for Chronic Constipation
Let's Discuss Some Solutions for Chronic Constipation
"Chronic constipation can have detrimental effects to daily life..."
Constipation is an extremely common symptom that has been reported to affect 63 million people in North America.1 Chronic constipation can have detrimental effects to daily life and is known to increase psychological distress and impair health related quality of life. Most commonly, individuals who are struggling with constipation often intervene with laxative use and dietary changes to increase fiber intake. These interventions fail to improve symptoms in about 50% of patients whom they are prescribed.2 If you find that you continue to struggle with constipation, there are many lifestyle changes one can adopt that can have a profound effect on symptoms including decreased frequency, straining, and pain with bowel movements.
Pelvic Floor Therapy for Bowel Urgency and Incontinence

Can pelvic floor therapy for bowel urgency and incontinence help you?
It's National IBS Month and our series on bowel health continues. Today’s article is for those with irritable bowel syndrome that tends towards softer stools and diarrhea (IBS-D). Most people have experienced fecal urgency at least once in their lives- the experience of rushing to the bathroom to have a bowel movement or having an accident.
Although management of conditions like irritable bowel syndrome should be multidisciplinary, pelvic floor therapy can play a role in regaining control of your bowel movements instead of allowing them control you.
Physical Therapy and Pilates for Urinary Incontinence and Low Back Pain

Let's Talk Pilates for Urinary Incontinence and Low Back Pain
"Physical Therapy is the first line of treatment for any type of urinary incontinence."
Incontinence, or unwanted urinary leakage, is commonly experienced by women, especially during pregnancy and postpartum. Experts often state, and research supports, it occurs in 1 in 3 women. While this may be common, it is not normal, and it is treatable! Physical therapy is the first line of treatment for any type of urinary incontinence. In fact, pelvic floor muscle training for women with stress urinary incontinence is six times more likely to result in a cure or a significant improvement. For all other types, women are twice as likely to report significant improvement or completely resolve their urinary incontinence. As you can imagine, getting help can dramatically improve their quality of life.
Tarlov Cyst: Physical Therapy and Treatment Options

Treatment Options for Tarlov Cyst: Physical Therapy
This article will go over what a Tarlov cyst is, what symptoms can arise from having a Tarlov cyst, how it is diagnosed, and common conservative and surgical treatments.
What is a Tarlov Cyst?
Tarlov cysts are sacral perineural cysts that consist of cerebrospinal fluid (CSF) close to the dorsal root ganglion on our sacral spine (the triangle shaped bone that connects to our tailbone). Tarlov cysts are often incidental findings on MRI’s, meaning most people with no symptoms may have Tarlov cyst(s). Paulsen, et al, looked at 500 MRIs of the lumbosacral spine and found an incidental rate of 4.6%; of which 20% were symptomatic. Approximately 1% of the cysts are large enough to cause compression, thus requiring prompt treatment.
Treating Bloating and Abdominal Distension: a Multi-Disciplinary Team
Why a Multi-Disciplinary Team is Best for Treating Bloating and Abdominal Distension
Bloating, abdominal distension, loose stools, constipation, abdominal or pelvic pain, fatigue, brain fog, weakness, nutritional deficiencies… these symptoms may be caused by a variety of gastrointestinal or pelvic conditions. If you are experiencing any of these symptoms, this article is a good place to start when deciding who to have on your care team, and what treatments can help!
Under the Radar: Physical Therapy for Urinary Incontinence - Part 1

Yes, Physical Therapy for Urinary Incontinence is a Thing
Urinary Incontinence Under the Radar: Part 1
November is Bladder Health Awareness month, and Femina PT would like to shine light on something that tends to go understated, unaddressed, brushed off as “normal”: urinary incontinence. This blog series focuses on the various effects that urinary incontinence (or UI) leaves on an individual’s life, and how conservative physical therapy treatment can help combat them. Lucky for you, reader, we love to talk about it.
The story goes like this - urinary incontinence is thought to be something expected with getting older, or something that occurs during pregnancy or as a result of delivery. Because of the embarrassment and shame that surrounds such issues, patients often don’t share these problems with their provider. Or worse, if they do share, they may be dismissed as their symptoms being a normal consequence of their stage of life. There is also a lack of awareness for conservative treatments such as pelvic floor physical therapy for these issues. Patients may fear surgery, medication, routine visits, and avoid talking about it all together. However, pelvic floor physical therapy for urinary incontinence can save patients time, money, and psychological distress. The numbers speak for themselves. Up to 45% of adults with bladder control problems fail to seek care.
Under the Radar: Urinary Incontinence and Physical Therapy - Part 2

More About Urinary Incontinence and Physical Therapy
Urinary Incontinence Under the Radar: Part 2
Welcome back for Part 2! November is Bladder Health Awareness month, and Femina PT would like to shine light on something that tends to go understated, unaddressed, brushed off as “normal”: urinary incontinence. In this blog series we’ve been addressing the various effects that urinary incontinence has on an individual’s life, and how conservative physical therapy treatment can help combat them. If you missed last week’s article, you can find it here.
Last week, we went over a lot of statistics. Urinary incontinence is without a doubt a healthcare crisis and places an enormous burden on the individual and their family members. Urinary incontinence, and the related sequelae, is expensive, isolating, and poses the risk of delirium, falls, pressure ulcers, and abuse.
What are Kegels?
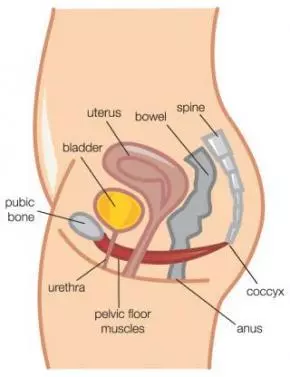
What are Kegels?
Kegels are a contraction of the pelvic floor muscles, sometimes referred to as “PC Contraction”. PC is short for “pubococcygeus”, the name of one of the many pelvic floor muscles.
However, after over a decade of practice, I have found that simply telling a patient to “Do Kegels” is usually not enough. Often, women perform pelvic floor exercises incorrectly, or do not do an amount appropriate for their strength levels. This finding has been confirmed by Bump et alin an August 1991 article from the American Journal of Obstetrics & Gynecology, “Assessment of Kegel pelvic muscles exercise performance after brief verbal instruction”.
What’s The Deal With Muscles And Potty Training? | Pediatric Blog Post

Muscles And Potty Training, What's the Connection?
Red flags to spot once your child starts potty training, how to prevent poor habits from forming, and when to see a pelvic floor physical therapist
Believe it or not children can show signs of a pelvic floor dysfunction like adults AND show similar signs and symptoms. Pelvic floor physical therapy is for anyone with a human body… these are the muscles that hold up our organs and prevent them from falling out (literally)! Pelvic floor dysfunctions can occur when the muscles of the pelvic floor have lost the ability to properly contact or fully relax.
Symptoms in children tend to become noticeable once potty training begins and have the potential to linger into their teens/ adulthood if gone untreated. It is important to pay attention to behaviors and poor habits that could indicate your child is having a tough time on the toilet.
Why you should be doing Kegels RIGHT NOW!

Wondering why you should be doing Kegels?
In my early days of being a pelvic floor PT, I was convinced I had the answer to all the woes of the pelvic floor. One word – Kegels. As I’ve developed professionally, I certainly realized Kegels have their place.
However, they do not have their place with all things related to the pelvic floor. There are specific instances when Kegels (also known as PC or pelvic floor muscle contractions) are the answer. I’m a firm believer in doing a Kegel program combined with a core strengthening program that will address the bigger picture. Here’s why you should be doing Kegels if you meet certain criteria:
Yoga Reduces Urinary Incontinence in Older Women

Learn How Yoga Reduces Urinary Incontinence in Older Women
A study presented at the annual meeting of the American Urological Association this past May of 2018 shows that a 3-month yoga intervention can reduce the frequency of urinary incontinence (UI) in women aged 50 years or older.
In the randomized trial completed by Dr. Alison Huang, MD and colleagues, a 3 month yoga therapy program was conducted with a group of 56 ambulatory women aged 50 years or older. These women had previously reported daily leaks and were not using any other clinical UI treatments.
The yoga program consisted of classes twice a week and one session of home practice weekly for three months. The therapeutic yoga classes were based out of the BKS Iyengar style of yoga.
After the three month trial, researchers saw a 74% decrease in daily leakage reported by the women in the yoga class. The women reported no negative outcomes related to the yoga practice.












