Treatment Options for Tarlov Cyst: Physical Therapy
This article will go over what a Tarlov cyst is, what symptoms can arise from having a Tarlov cyst, how it is diagnosed, and common conservative and surgical treatments.
What is a Tarlov Cyst?
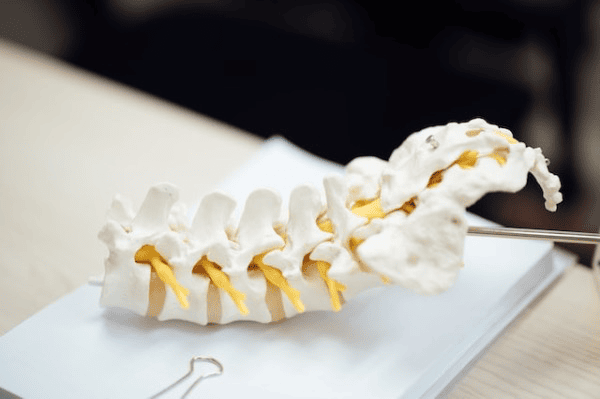
Tarlov cysts are sacral perineural cysts that consist of cerebrospinal fluid (CSF) close to the dorsal root ganglion on our sacral spine (the triangle shaped bone that connects to our tailbone). Tarlov cysts are often incidental findings on MRI’s, meaning most people with no symptoms may have Tarlov cyst(s). Paulsen, et al, looked at 500 MRIs of the lumbosacral spine and found an incidental rate of 4.6%; of which 20% were symptomatic. Approximately 1% of the cysts are large enough to cause compression, thus requiring prompt treatment.
What are the symptoms of a Tarlov Cyst?
Some people have Tarlov cysts with symptoms, and some have Tarlov cysts with no symptoms. Depending on the size and location of the cyst, it can affect the nerve roots coming out of the spine. The most common location of the tarlov cysts is on the second sacral vertebrae. The sizes of the cysts range, on average, from 1-2 centimeters. This is a big area where very important nerves live, such as the pudendal nerve, sciatic nerve, and many others. Our pudendal nerve is responsible for sensation of our perineum (saddle region), bladder/bowel function, and volitional control of the muscles of our pelvic floor. Another big nerve is the sciatic nerve and this innervates the muscles of the back of the thighs and indirectly innervates the lower legs. Because of the location of the cyst, you can imagine that Tarlov cysts can lead to low back pain, leg pain, pelvic pain, sensory disturbances and bladder/bowel dysfunction.
Common symptoms are:
- Low back pain
- leg pain
- pain from sitting to standing
- numbness/sensory dysfunction
- Urinary urgency/urinary frequency
- sexual dysfunction
Baker, et al. studied bladder findings in those with symptomatic Tarlov cysts and that also underwent urodynamic testing. The authors found an earlier sensation of bladder filling, involuntary detrusor (bladder muscle) contractions, urethral instability, and stress urinary incontinence. As you can see, Tarlov cysts can have quite an influence on our urogenital function.
How are Tarlov Cysts diagnosed?
Often Tarlov cysts are diagnosed through MRI, CT, or myelogram of the lumbosacral spine. If it is suspected to be the cause of your pain/symptoms, often a CT guided percutaneous aspiration of the cyst is performed to see if short-term relief occurs, and goes into consideration as a surgical candidate.
Treatment Options for Tarlov Cysts
Conservative treatments can include analgesic medications, non-steroid anti-inflammatory medications, and physical therapy. Physical therapy would focus on the individual symptoms, help with pain management and possibly introduce light strengthening of muscles that may have gotten weaker as a result of the cyst.
Tarlov Cyst Disease Foundation listed some wonderful general suggestions:
- Avoid heavy lifting, straining or pulling that may increase pressure on low back
- ice and/or heat packs on low back
- minimize prolonged periods of sitting or standing (possibly apply sitting cushions that help decrease pressure on perineum).
- avoid constipation as that can increase pressure on cyst while straining (check out our other blogs on how to help manage constipation:
- Pain management, including TENS
Furthermore, pelvic floor physical therapists can help with constipation, go over toileting posture and mechanics, bladder symptoms (urinary incontinence, inc. urinary frequency/urgency, or difficulty with urinating), sitting posture/strategies, standing posture/strategies and apply pain management techniques including light manual therapy and therapeutic exercises.
SURGICAL TREATMENTS:
There are many different surgical techniques to help should conservative methods fail or symptoms worsen. Different neurosurgical techniques include: cyst fenestration, cyst shrinkage, partial excision and oversewing of cyst’s wall with or without nerve root repair, and complete excision of the cyst with the nerve root. Although surgery provides relief for many, including a significant reduction in pain, improvement in bladder/bowel function and sexual function, there can be some complications and in some circumstances, may be recurrence of cyst with a return of symptoms. Please go to tarlovcystfoundation.org to help you find a neurosurgeon that can help guide you through this journey.
References:
- Xu J, Sun Y, Huang X, Luan W (2012) Management of Symptomatic Sacral Perineural Cysts. PLoS ONE 7(6): e39958. doi:10.1371/journal.pone.0039958
- Baker M, Wilson M & Wallach S. (2018). Urogenital symptoms in women with Tarlov cysts. J Obstet Gynaecol Res 44(9): 1817-1823. doi:10.1111/jog.13711.
- “FAQs.” Tarlov Cyst Disease Foundation. https://www.tarlovcystfoundation.org/faqs/.
- Medani K, Lawandy S, Schrot R, et al. Surgical Management of symptomatic Tarlov cysts: cyst fenestration and nerve root imbrication – a single institutional experience. J Spine Surg 2019;5(4):496-503 | http://dx.doi.org/10.21037/jss.2019.11.11