Alphabetical Index of Articles on Women's Sexual, Pelvic Floor, and Reproductive Health
How Do I Know If I Have A Weak Pelvic Floor?

In this article we’ll discuss how to assess if you may have a weak pelvic floor, what symptoms are and basic orientation to the pelvic floor.
What is the pelvic floor?
The pelvic floor is a very important group of muscles that live in the bottom of the pelvis. Both men and women have a pelvic floor. These muscles sit in the bottom of the pelvic floor like a hammock, and can move up and down like a trampoline to support your internal organs inside your body. They also help to control the openings and closures in the bottom of the pelvis, which is why they are so essential to urinary, bowel and sexual function. Just like any muscle, when they are weak, they can start to cause issues with any of these functions. Common signs of a weak pelvic floor include urinary incontinence, fecal (or bowel) incontinence, feeling of pelvic heaviness or pelvic organ prolapse, as well as low back or hip pain.
How Obesity Increases Urinary Incontinence

Learn How Obesity Increases Urinary Incontinence and How Pelvic Floor Therapy Can Help
Urinary Incontinence is common, why suffer?
Urinary incontinence is the loss of bladder control.Urinary incontinence affects up to 1 in 3 women. The two most common types of urinary incontinence that affect women are stress incontinence and urge incontinence (also called overactive bladder, or OAB). Incontinence affects twice as many women as men. This may be because pregnancy, childbirth, and menopause are contributing factors to urinary incontinence. Urinary incontinence should not be considered a normal part of aging, and it can be treated.
A new article published in September, 2018 by Lamerton, Torquati, & Brown found that being overweight (BMI 25-30) increased risk of urinary incontinence for young and middle aged by 35% and obesity (BMI ≥30) almost doubles the risk at 95%.
Incontinence
Incontinence is the inability to control bodily functions resulting in the loss of urine or feces.
Physical therapy treatments are important to restore the normal bladder and bowel functions through strengthening, use of behavioral modification strategies, correction of faulty patterns and habits and use of biofeedback and electrical stimulation as appropriate to enhance pelvic floor rehabilitation.
Types of incontinence include:
The Latest in the Treatment of Urinary Incontinence

The latest literature review conducted by Mazur-Bialy et al. (2020) shows the most modern methods of pelvic floor physical therapy that can help with urinary incontinence.
Here at Femina PT, we pride ourselves in keeping up with the current best practices and latest techniques. Here’s a breakdown of the latest techniques and how we utilize them at the clinic.
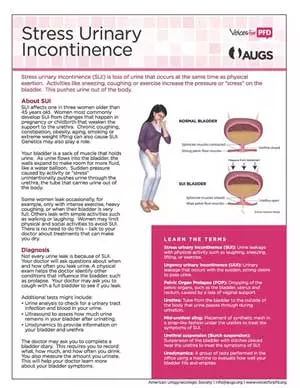
What is urinary incontinence?
Urinary incontinence refers to the involuntary loss of urine, which can range from a few drops (also called light bladder leakage) to complete loss that wets the floor. There is actually more than one kind of urinary incontinence: the two most common types of urinary incontinence that affect women are stress incontinence and urge incontinence (also called overactive bladder, or OAB).
Yoga Reduces Urinary Incontinence in Older Women

Learn How Yoga Reduces Urinary Incontinence in Older Women
A study presented at the annual meeting of the American Urological Association this past May of 2018 shows that a 3-month yoga intervention can reduce the frequency of urinary incontinence (UI) in women aged 50 years or older.
In the randomized trial completed by Dr. Alison Huang, MD and colleagues, a 3 month yoga therapy program was conducted with a group of 56 ambulatory women aged 50 years or older. These women had previously reported daily leaks and were not using any other clinical UI treatments.
The yoga program consisted of classes twice a week and one session of home practice weekly for three months. The therapeutic yoga classes were based out of the BKS Iyengar style of yoga.
After the three month trial, researchers saw a 74% decrease in daily leakage reported by the women in the yoga class. The women reported no negative outcomes related to the yoga practice.












