Urogenital & Pelvic Organ Prolapse: What It Is, Symptoms, and How Physical Therapy Can Help
Pelvic organ prolapse is a common yet often misunderstood condition that affects many people, especially women, over time. If you’ve ever felt a heavy sensation, noticed a bulge, or experienced urinary difficulties, pelvic organ prolapse symptoms could be the cause. The good news is that pelvic organ prolapse treatment doesn’t always require surgery—conservative, non-surgical interventions can be highly effective. At FeminaPT, our experienced pelvic floor physical therapists specialize in addressing this condition with a personalized care plan. In this service page, we’ll explain what urogenital & pelvic organ prolapse is, the different types, typical causes, symptoms to watch for, and how physical therapy can help restore function and comfort. Whether you’re exploring treatment options or seeking to prevent worsening of prolapse, this guide will help you understand your path forward.
What is Urogenital & Pelvic Organ Prolapse
Urogenital & pelvic organ prolapse (often abbreviated POP) refers to a weakening of the support structures—muscles, ligaments, connective tissue—that normally hold pelvic organs in their proper positions. When these supports are compromised, one or more pelvic organs may drop or bulge downward into or through the vaginal canal or towards the vaginal opening. This may involve organs like the bladder, uterus, small intestine, or rectum.
Pelvic organs are supported by the pelvic floor, ligaments, and connective tissue. When these weaken—due to childbirth, hormonal changes, aging, or increased abdominal pressure—pelvic organ prolapse can occur, causing the bladder, uterus, or rectum to shift downward. It’s not only about a visible bulge but also about function: how well you control these organs and how your core and posture support the pelvic floor. Mild prolapse may cause a few issues, but symptoms often worsen over time. Treatment focuses on restoring support, improving muscle coordination, and easing symptoms. Non-surgical care, including specialized physical therapy like that offered at FeminaPT, is highly effective, with options such as pessaries, lifestyle changes, or surgery for advanced cases.
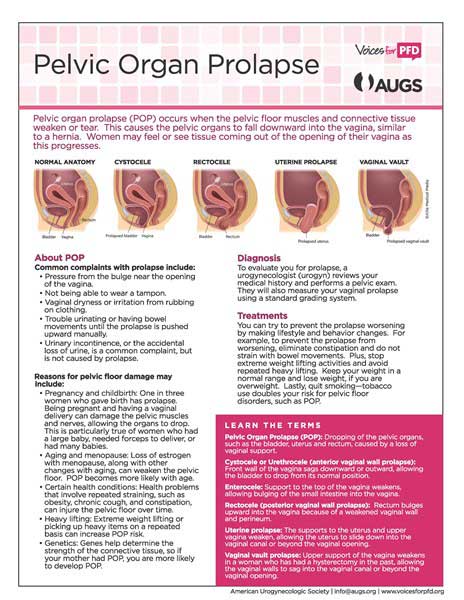
Types of Urogenital & Pelvic Organ Prolapse
At Femina Physical Therapy, we recognize several major types of prolapse. Each affects a different part of the pelvic organ system and may produce unique symptoms. Understanding the type helps tailor the most effective pelvic organ prolapse treatment plan.
Here are the main types:
- Urethrocele – prolapse of the lower anterior vaginal wall involving the urethra. This may lead to urinary problems and a sense of pressure at the front of the vagina.
- Cystocele—prolapse of the upper anterior vaginal wall, typically involving the bladder. This is one of the more common types; people may notice a bulge, difficulty emptying the bladder, or urinary frequency or urgency.
- Uterovaginal prolapse—descent of the uterus and cervix into or toward the upper vaginal canal. Depending on severity, it can lead to visible bulging and discomfort with standing or during intercourse.
- Enterocele—prolapse of small bowel (intestine) into the upper posterior wall of the vagina. This type may lead to pelvic-pressure sensations and sometimes issues with bowel function.
- Rectocele – prolapse of the lower posterior vaginal wall involving the rectum. People with rectocele often feel fullness or a bulge in the back wall of the vagina, difficulty with bowel movements, or incomplete evacuation.
Severity of each type can also vary (from mild descent to more serious bulging), and sometimes more than one type co-exists in the same individual.
Causes of Urogenital & Pelvic Organ Prolapse
Multiple factors contribute to the development of pelvic organ prolapse. Here are some of the most common causes identified by research and clinical practice at FeminaPT:
- Childbirth trauma: Vaginal delivery (especially with forceps or vacuum use), large baby, long second stage, tearing or episiotomy, or levator ani muscle injury (levator ani avulsion) all increase risk.
- Aging and hormonal changes: With menopause, estrogen levels decrease, connective tissues weaken, collagen becomes less resilient, and overall pelvic support diminishes. feminapt.com+1
- Genetic predisposition and connective tissue differences: Some people are born with or develop weaker connective tissue or familial traits that make them more prone to prolapse. feminapt.com
- Increased intra-abdominal pressure: Chronic coughing, obesity, heavy lifting, straining with bowel movements, or high-impact exercise can cumulatively strain the pelvic floor supports.
- Poor posture, core instability, or weak support muscles: Weak core muscles, imbalance between muscles (e.g., weak versus tight muscles), and poor biomechanics during movement or lifting all play a role.
- Post-surgical or injury-related damage: Surgery in the pelvic or abdominal region, scar tissue or adhesions, or trauma can weaken or distort the support structure.
Symptoms of Urogenital & Pelvic Organ Prolapse
Symptoms can vary widely depending on the type, severity, and individual body. Some people may have minimal symptoms, while others feel constant discomfort. Here are the most commonly reported pelvic organ prolapse symptoms:
- A feeling of heaviness or pressure in the pelvis, vagina, or lower abdomen
- A bulge or visible protrusion at or near the vaginal opening, or feeling something is “falling out” or “droopy.”
- Urinary symptoms: incontinence, urgency, frequency, and difficulty emptying the bladder completely.
- Bowel symptoms: difficulty with bowel movements, need to strain, sense of incomplete evacuation (especially with rectocele or enterocele).
- Discomfort or pain with sexual intercourse, vaginal sensitivity, or pain during or after activity or heavy lifting
- Pelvic, lower back, or hip discomfort that worsens with standing, lifting, prolonged activity, or at the end of the day.
- Sometimes visible or palpable changes: you might notice the tissue when wiping, or feel the bulge with increased intra-abdominal pressure (coughing, sneezing, straining).
How Pelvic Floor Physical Therapy Can Help in Treating Urogenital & Pelvic Organ Prolapse
At FeminaPT, physical therapy is central to managing pelvic organ prolapse—whether your goal is to prevent progression, ease symptoms, or avoid surgery. Our specialists evaluate the entire support system, including the pelvic floor, core, connective tissues, posture, and movement patterns, to design a personalized treatment plan. Depending on your unique needs, we often combine multiple approaches for the best results.
Here are several ways Pelvic Floor Physical Therapy at FeminaPT can help treat urogenital & pelvic organ prolapse:
- Posture & Body Mechanics Training—improving how you sit, stand, lift, and bend so your pelvic organs get more support and less strain. This helps reduce pressure on weakened tissues and slows progression of prolapse.
- Diastasis Recti Recovery / Core Stabilization—restoring separation of the abdominal muscles to improve core control, which supports pelvic organ position. FeminaPT uses targeted exercises to strengthen the transverse abdominis and other core muscles to support the pelvic floor.
- Regaining Pelvic Floor Strength, Function & Flexibility—exercises and tailored interventions to improve the strength and elasticity of pelvic floor muscles, allowing them to better hold up organs and adapt to daily loads. Trainers assess tone and coordination to develop individualized programs.
- Breath Control & Proper Body Mechanics—using diaphragmatic breathing and movement strategies to reduce downward pressure during everyday tasks like lifting or coughing, helping protect prolapsed organs. FeminaPT emphasizes alignment and breath-movement coordination.
- Movement Retraining Including Core & Pelvic Floor Coordination—working on how your core, hips, and pelvic floor move together for greater overall stability. This helps in performing daily activities without aggravating prolapse.
- Education & Home Strategies—helping clients understand what behaviors (e.g., heavy lifting, straining, cough control) exacerbate prolapse and how to modify them. Also includes awareness of pelvic organ positioning, toileting habits, and consistency in home exercise.
Treatment Options at Femina Physical Therapy
At Femina Physical Therapy, we offer a comprehensive range of treatment options for pelvic organ prolapse, combining non-surgical interventions, targeted exercises, and lifestyle strategies. Our goal is to reduce symptoms, restore function, and support long-term pelvic health through personalized, evidence-based care.
- Pessary Fittings—We fit pessaries—supportive devices inserted into the vagina—to help reduce the discomfort, bulge, and urinary symptoms that often accompany pelvic organ prolapse. They provide structural support and can be especially helpful as a non-surgical option.
- Pelvic Floor Strength Training—Targeted strengthening of the pelvic floor muscles to improve your ability to support pelvic organs. At FeminaPT, therapists identify weak areas and prescribe exercises (in-office and at home) to build strength, endurance, and function.
- Functional Training—Exercises that incorporate coordination, balance, and strength into everyday movements. We help you adapt body mechanics for lifting, posture, breathing, and other functional tasks to reduce strain on pelvic supports.
- Manual Therapy—Skilled hands-on techniques to address short or tight muscles, fascia restrictions, scar tissue, adhesions, or other soft tissue dysfunctions that may compromise pelvic organ support. Manual therapy helps improve tissue mobility and reduce tension.
- Biofeedback—Using biofeedback devices to give visual or auditory feedback about how your pelvic floor muscles are contracting, relaxing, and coordinating. This helps you “Find” the muscles, improve awareness, and perform effective exercises.
- Electrical Stimulation—In cases where muscles are weak or it is difficult to contract them voluntarily, electrical stimulation can help “wake up” these muscles, improve activation, and assist in strengthening. It’s a pain-free modality that supports other treatments.
- Lifestyle & Behavioral Education—We coach patients in posture, body mechanics, lifting with care, managing intra-abdominal pressure (avoid straining), breath control, bladder and bowel habits, weight management, and strategies to reduce aggravating behaviors.
- Therapeutic Exercises Beyond the Pelvic Floor—Strong core muscles, hip, back, and connective tissue function all influence pelvic organ support. We include exercises that target the hips, low back, and abdominals (including those with diastasis recti when present) to stabilize the core and support overall pelvic health.
- Pre- and Post-Surgical Rehabilitation—For people considering surgery (or those who have had surgery), physical therapy before and after surgery can improve outcomes, reduce symptoms, support recovery, and help prevent recurrence of prolapse.
- Continued Monitoring & Maintenance—As with many musculoskeletal and pelvic health conditions, maintenance matters. We provide follow-up, adjust treatment as needed, and support long-term strategies to prevent symptom return.
This combination of treatments is customized based on the type(s) of prolapse you have, your symptom severity, your lifestyle demands, and your goals. We aim to reduce discomfort, improve function, and restore quality of life without unnecessary risk.
Frequently Asked Questions
Here are some common questions about pelvic organ prolapse, its symptoms, and treatment. If you don’t see your question below, please reach out to our team for personalized guidance.
- Can pelvic organ prolapse get better without surgery? – Yes. Many people benefit from pelvic floor physical therapy, pessary use, lifestyle modifications, and strengthening. For mild to moderate prolapse, non-surgical pelvic organ prolapse treatment often reduces symptoms significantly and may prevent progression.
- What are the risk factors for developing pelvic organ prolapse? – Key risk factors include childbirth (especially vaginal delivery), older age, hormonal changes (e.g., menopause), obesity, chronic straining (bowel or cough), connective tissue weakness, and certain postural or biomechanical stresses.
- What should I expect in a physical therapy evaluation for prolapse? – During the evaluation, a therapist will assess pelvic floor muscle strength, coordination, endurance, mobility of surrounding tissues, posture, and core behavior around bowel and bladder habits and movement patterns. Expect a personalized care plan with both in-clinic sessions and home exercises.
- How long does treatment take to see improvement? – Improvement timing varies by individual, severity, consistency, and how many treatment components are used. Many patients notice symptom relief (less bulging, reduced heaviness, improved bladder control) in a few weeks of therapy and more significant changes over a few months of consistent work.
- Will doing pelvic floor exercises (like Kegels) be enough? – Pelvic floor muscle training (PFMT) is foundational, but it often works best when combined with other interventions: manual therapy, biofeedback, behavior change, managing pressure, and training of supporting musculature. Some individuals need extra support (like pessaries or electrical stimulation).
- Are there things I should avoid if I have prolapse? – Yes. Avoid heavy lifting without support, high-impact exercises that increase intra-abdominal pressure if not properly managed, straining with bowel movements, holding in breath during exertion, or ignoring symptoms. Also, improper posture and movement patterns can worsen prolapse symptoms.
- When should I consider surgery? – Surgery may be considered if non-surgical pelvic organ prolapse treatment does not relieve symptoms, or if the prolapse is severe, significantly impacting quality of life, or risks complications. Physical therapy is often useful both before and after surgery to improve outcomes and reduce recurrence.

