May is Osteoporosis Awareness Month.
Did you know that Physical Therapists are an essential member of your interdisciplinary care team?
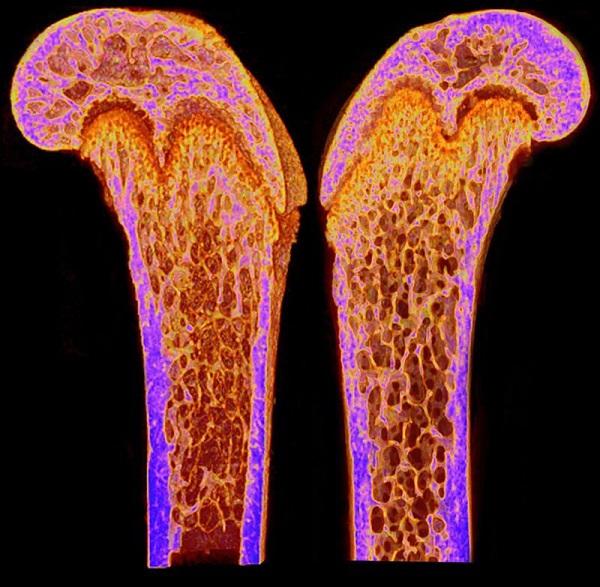
With life expectancy increasing it is becoming more evident that bone health and fall prevention are key to a good quality of life. Osteoporosis is defined as a decrease in bone mass or a change in the structure of the bone causing the bone to be more fragile.1 If the bone is weak there is a higher chance of a fracture (bone break). The most common areas of fractures are the hip, spine, forearm, and humerus (upper arm bone). Osteoporosis causes more than 8.9 million fractures annually worldwide, affecting predominantly postmenopausal women. The probability of women, at menopause, of having an osteoporotic fracture exceeds that of breast cancer and the likelihood of a fracture is approximately 40%.2
Bone mineral density is measured through a scan called a Dual-Energy X-ray Absorptiometry (DEXA). It can be used to measure the bone mineral density of the whole skeleton as well as specific sites. Approximately 21% of women aged 50–84 years are classified as having osteoporosis.2
Risk factors for osteoporosis are:
- Sex--Women are more likely to develop osteoporosis
- Age--risk increases with age
- Race--Caucasian and Asian descent have a higher chance
- Family History--having a parent or sibling with osteoporosis
- Body frame--smaller frames have a higher chance as they have less bone to draw from as they age
- Lowered sex hormones ie. postmenopausal women with decreased estrogen
- Increased thyroid hormones can increase risk
- Low calcium intake
- Long term use of corticosteroids
- Certain medical conditions have a higher chance of developing osteoporosis
- Celiac disease
- Inflammatory bowel disease
- Kidney or liver disease
- Cancer
- Multiple myeloma
- Rheumatoid arthritis

Additionally, lifestyle choices can affect the risk of developing osteoporosis:
- Sedentary lifestyle: Patients that are confined to a bed can lose as much bone in one week that they would otherwise lose in a whole year.2 For thisreason, it is always important to be as active as possible. The most beneficial exercises are weight-bearing exercises that focus on balance and good posture--and physical therapists are your ideal health care partner to address these needs.
- Excessive alcohol consumption: More than two alcoholic drinks a day increases the risk of osteoporosis.
- Tobacco use: Tobacco is a toxin to bone and regular use can lead to weak bones.
The important take-home message is to try and modify the risk factors that you have control over, especially if you have genetic factors or medical conditions that increase your risk. The consequence of having osteoporosis is a higher chance of developing a fracture. An osteoporotic fracture can be characterized if it results from a low-energy fall. Low energy is defined as a fall from a standing height or less, or trauma that in a healthy individual would not cause a fracture.3 It is important to understand your fall risk and make sure to modify factors to increase your safety and prevent a fall. A physical therapist has a variety of fall risk assessment tests they can administer to provide patients with a quantifiable measure of their fall risk. A physical therapist can also provide a specific exercise program that is individualized based on the type of balance deficit found on your initial or subsequent visits. It is also important to modify the home environment for safety.
Modifiable factors for fall risk:
- Increasing lighting at night: night lights or turning the light on when using the restroom
- Speaking with your doctor about decreasing or changing medications that alter balance and alertness
- Removing all rugs (as these can be a tripping hazard)
- Use of handrails next to steps
- Removing all obstacles and items off the floor
- Slippery floors5

How can you prevent osteoporosis?
Primary prevention of osteoporosis:
The goal is to reach your maximal bone mass and decrease the loss of bone in the early adult years. Women usually reach their peak bone mass at age 30
Secondary prevention:
The focus is to prevent fractures in women who have osteopenia or osteoporosis. Most of the women in this stage are considered peri or postmenopausal.
Tertiary prevention:
In this strategy the goal is to prevent future fractures in women who have already had at least one fracture.
There is extensive evidence supporting exercise to improve bone health and balance performance. Although, it has been shown that excessive rigorous training and restrictive diets in elite athletes can have detrimental effects on bone density. Several different types of exercise have been shown to be beneficial for maintaining and even improving bone density. A large study used specific yoga postures that were modified to be safe with patients that have osteoporosis. Some of these adaptations were avoiding end range of motion for the hips and spine. After the participants participated in a 12 min yoga routine for two years they measured increased bone density in the spine, hips and femur.8 A meta-analysis of exercise interventions--resistance-alone versus combined resistance training with high impact weight-bearing exercise--was compared. The results of the study suggest the combined intervention was most effective at improving bone mineral density at the hips and lower spine.9 Pilates can also be an effective exercise to increase bone mass in postmenopausal women when compared to a control group without an exercise program.10
References
- Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, et al. (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8: 136
- Strom O, Borgstrom F, Kanis JA, Compston JE, Cooper C, McCloskey E, Jonsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos doi:10.1007/s11657-011-0060-1
- Kanis JA, Johnell O, Oden A, Dawson A, De Laet C, Jonsson B (2001) Ten year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int 12:989–995
- Bonaiuti D, Shea B, Iovine R, Negrini S, Robinson V, Kemper HC, Wells G, Tugwell P, Cranney A (2002) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev CD000333
- Michael YL, Whitlock EP, Lin JS, Fu R, O'Connor EA, Gold R (2010) Primary care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 153:815–825
- Rizzoli R (2008) Nutrition: its role in bone health. Best Pract Res Clin Endocrinol Metab 22:813–829
- Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32: 468–73
- Lu, Yi-Hsueh PhD; Rosner, Bernard PhD; Chang, Gregory MD, PhD; Fishman, Loren M. MD, B Phil (oxon.) Twelve-Minute Daily Yoga Regimen Reverses Osteoporotic Bone Loss, Topics in Geriatric Rehabilitation: April/June 2016 - Volume 32 - Issue 2 - p 81-87 doi: 10.1097/TGR.0000000000000085
- Zhao, R., Zhao, M. & Xu, Z. The effects of differing resistance training modes on the preservation of bone mineral density in postmenopausal women: a meta-analysis. Osteoporos Int 26, 1605–1618 (2015). https://doi.org/10.1007/s00198-015-3034-0
- Angın, Ender, Erden, Zafer, and Can, Filiz. ‘The Effects of Clinical Pilates Exercises on Bone Mineral Density, Physical Performance and Quality of Life of Women with Postmenopausal Osteoporosis’. 1 Jan. 2015 : 849 – 858.
- “Osteoporosis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 21 Aug. 2021, https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968.