
The Femina Physical Therapy Blog
Featuring original articles by our staff about current events and trends
Explore our insightful blog articles on pelvic health, where we delve into essential topics that empower and educate. From understanding pelvic floor disorders to strategies for conquering infertility, our content is designed for those seeking knowledge and support. We discuss the latest research, expert advice, and practical tips to enhance your well-being and foster a deeper connection to your body.
Featured From the Blog:
Postpartum Sexuality & Mood Changes in Women with Pelvic Girdle Pain

Does my pelvic girdle pain have anything to do with my mood and sexuality?
Many of our patients experience sexual dysfunction and anxiety, depression and chronic pain. These conditions are known to coexist, and we unpack each component of pain, mood and one’s behaviors, desires and attitudes related to sex and physical intimacy.
Pelvic girdle pain is defined as “pain between the posterior iliac crests and gluteal folds particularly in the vicinity of the sacroiliac joint” (Simonds). More simply stated: in the very low area of your back and buttock. Pelvic girdle pain is common postpartum and may impact disability in the fourth trimester. Many are aware of peripartum symptoms such as low back pain, incontinence, pelvic organ prolapse, pain with intercourse, and postpartum depression. Knowing that many women experience pain during and after pregnancy - what can we learn about the effects of pelvic girdle pain? Specifically, what impact does pelvic girdle pain have on symptoms of mood and sexuality?
Read more: Postpartum Sexuality & Mood Changes in Women with Pelvic...
Treating Bloating and Abdominal Distension: a Multi-Disciplinary Team
Why a Multi-Disciplinary Team is Best for Treating Bloating and Abdominal Distension
Bloating, abdominal distension, loose stools, constipation, abdominal or pelvic pain, fatigue, brain fog, weakness, nutritional deficiencies… these symptoms may be caused by a variety of gastrointestinal or pelvic conditions. If you are experiencing any of these symptoms, this article is a good place to start when deciding who to have on your care team, and what treatments can help!
Understanding Relaxin: Why It Doesn’t Cause Pain in Pregnancy

Pregnancy is a time of significant physical and hormonal changes, and among the many hormones involved, Relaxin plays a crucial role. However, there’s a common misconception that Relaxin is responsible for pain during pregnancy. Let’s take a closer look at what Relaxin does and why it doesn’t directly cause pain.
What is Relaxin?
Relaxin is a regulatory hormone involved in growth, metabolism, and tissue remodeling after an injury to our bones, ligaments, muscles or tendons (Dehghan 2014). During pregnancy, Relaxin levels begin to increase in the first trimester to help the body prepare for childbirth by relaxing the ligaments in the pelvis and softening the cervix (Aldabe 2012, Daneau 2014). The ligaments of the pelvis will begin to relax around the 10th-12th week of pregnancy (Aldabe 2012). This process allows for greater flexibility in the pelvic area, facilitating delivery and accommodating the growing baby.
Read more: Understanding Relaxin: Why It Doesn’t Cause Pain in...
- Details
- Written by: Staff
- 28384 Views
Self Care After Cesarean Section, With an Emphasis on Baby Care Ergonomics
Today we talk about ergonomics with baby care after a cesarean section. It’s important for all new parents to conserve energy and protect their own bodies while adjusting to the care of a new baby, especially those who have had a cesarean. Today we will discuss body mechanics of picking up a baby, breastfeeding, and the like after a C-Section.
Lifting Restrictions
As a cesarean section is an abdominal surgery, your doctor will likely advise you to not lift anything over 8-10 lbs, depending on the doctor as well as the details regarding your cesarean and your personal health. Lifting restrictions typically last anywhere from 6-8 weeks. This may prevent you from lifting household items heavier than a gallon of milk… That means no carrying baskets of laundry or heavy bags of groceries.
Read more: Ergonomics with Baby Care and Self Care After Cesarean...
- Details
- Written by: Staff
- 16439 Views
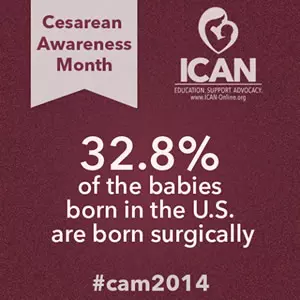
Learn To Do Cesarean Section Early Recovery Exercises
It’s Cesarean Section Awareness Month!
Trauma to the body is something all who give birth to a baby experience. With those who deliver via cesarean (c-section), there is the added trauma of an abdominal surgery in addition to the trauma of labor and delivery.
Today we will talk about post-delivery rehabilitation, with an emphasis for those who have had a cesarean. This information is all about self care to recover birth and is useful for ALL new mothers, whether delivering via the vaginal canal or a cesarean section.
In an upcoming blog post this month, we will discuss body mechanics of picking up a baby, breastfeeding, and the like after a C-Section.
- Details
- Written by: Staff
- 12817 Views

Can pelvic floor therapy for bowel urgency and incontinence help you?
It's National IBS Month and our series on bowel health continues. Today’s article is for those with irritable bowel syndrome that tends towards softer stools and diarrhea (IBS-D). Most people have experienced fecal urgency at least once in their lives- the experience of rushing to the bathroom to have a bowel movement or having an accident.
Although management of conditions like irritable bowel syndrome should be multidisciplinary, pelvic floor therapy can play a role in regaining control of your bowel movements instead of allowing them control you.
Read more: Pelvic Floor Therapy for Bowel Urgency and Incontinence
- Details
- Written by: Staff
- 12169 Views

Dealing With Chronic Constipation? Read On.
Most people experience constipation from time to time. Constipation isn’t just the inability to have a bowel movement, it includes the difficulty associated with bowel movements. Travel, inactivity, illness, and certain over the counter medications taken “as needed” commonly result in short-term or acute constipation. Constipation lasting longer than three months is considered chronic constipation. Chronic constipation should be treated by a doctor to prevent health complications.
Clear communication is essential to working with doctors, but the general public often has only a rudimentary understanding of medical terms - including constipation. There is often a gap between the physician and the patient’s perception of constipation which can lead to confusion. (1, 2, 7, 10) A study of people who thought they had constipation showed that only a third actually fit the criteria for constipation, while the rest actually had Irritable Bowel Syndrome or other gastrointestinal disorders. (9) So what are the criteria for constipation?
- Details
- Written by: Heather Jeffcoat, DPT
- 8382 Views

A Conversation about Female Sexual Health & Pelvic Pain
with Screening of Animated Short Film "Tightly Wound"
Femina PT, the Pelvic Health and Rehabilitation Center, and the Milli, the first Expandable Dilator, are teaming up to bring Shelby Hadden and her animated short film about vaginismus, Tightly Wound, to Los Angeles on Saturday, May 19th! Many of you may know of Shelby and her past struggles with pelvic pain. Her journey getting diagnosed and treated combined with her skills as a filmmaker inspired her to create Tightly Wound to help raise awareness about vaginismus and pelvic pain, helping women get diagnosed and get the help they need.
Read more: You Are Invited to Becoming unWOUND: A Conversation About...
- Details
- Written by: Heather Jeffcoat, DPT
- 7911 Views

Tips for Teaching Your Daughters About Endometriosis
Endometriosis affects 1 in 10 women and girls. The delay for diagnosis averages 7 years! How early should you start the discussion about this debilitating condition? As a pelvic health physical therapist, I believe this conversation should start not long after your daughter begins menstruating. As moms, we need to be aware about what is “normal” versus “abnormal”. We only know if we ask them questions. It can be a scary time for girls when they first get their periods, and it can be devastating if there is a lot of pain. We need to be a strong support system for our daughters, but also educate them on the norms.
Is it normal to have cramping? Yes. It’s the uterus contracting to shed the lining of the uterus. Mild to moderate cramping can often be helped with Motrin, heating pads, gentle exercise and adequate hydration. Be careful to not dismiss her if she comes to you complaining of severe cramping during her cycle. If her pain is so severe she is vomiting, please do not accuse her of being “too dramatic”. I’ve heard these stories in my office from my patients as they relay their history and how long they complained of severe pain, only to be accused of playing up their pain too much. It only delayed their treatments and added psychological factors as they were made to feel that their pain wasn’t that bad or worse…not real at all.
- Details
- Written by: Staff
- 7410 Views
How Does Endometriosis Affect Fertility and Pregnancy?
As we continue our series about endometriosis, today we address how endo might affect fertility and pregnancy.
Endometriosis Does Not Equal Infertility
Having endometriosis does not automatically mean that you will never have children. What it does mean is that you might have more trouble getting pregnant. About 30% of those with endometriosis have trouble with fertility and struggle to get pregnant. Others with endometriosis have no difficulty getting pregnant, or eventually get pregnant after utilizing medical interventions including surgery to remove endometrial growths, or reproductive technologies like in vitro fertilization to help with conception.
Read more: Does Endometriosis Affect Fertility and Pregnancy?
- Details
- Written by: Staff
- 50616 Views

Yoga Poses to Ease Pelvic Pain
Also Effective for Endometriosis Pain
1 in 10 women have endometriosis and experience different forms of pain—pain with urination, pain with bowel movements, painful periods, pelvic pain, ovulation pain, painful sex, abdominal pain, and nerve pain. The Office on Women’s Health of the U.S. Department of Health and Human Services estimates 5 million American women are affected by endometriosis.
As we covered in a previous blog post, endometriosis is a condition where endometrial-like tissue grows outside of the uterus (endometrial tissue is tissue that usually tissu grows inside of the uterus). Endometrial-like tissue can implant on the surface of organs and structures including the ovaries, bladder, rectum, and along the walls of the abdomen and pelvis. These tissues can cause inflammation and pain to develop throughout the abdomen and pelvic cavity.
Read more: Yoga Poses to Ease Pelvic Pain and Endometriosis Pain












