
The Femina Physical Therapy Blog
Featuring original articles by our staff about current events and trends
Explore our insightful blog articles on pelvic health, where we delve into essential topics that empower and educate. From understanding pelvic floor disorders to strategies for conquering infertility, our content is designed for those seeking knowledge and support. We discuss the latest research, expert advice, and practical tips to enhance your well-being and foster a deeper connection to your body.
Featured From the Blog:
Running Mechanics and Pelvic Floor Health: The Impact of Footwear

Did You Know That Proper Footwear Can Improve Your Running Mechanics and Pelvic Floor Health?
How Do My Feet Impact My Pelvic Floor When I Run?
If you are a runner, you tend to look for ways to improve your running. If you’re thinking about starting up or returning to running, it can feel intimidating particularly if you have any symptoms related to pelvic floor dysfunction. This only complicates an exercise that, on the surface, seems fairly straight forward. There are some studies that have looked at how your feet can play a part in your pelvic floor muscle function while you run. And if you are looking to return to running postpartum, read on and also check out this article by one of our pelvic floor physical therapists.
Read more: Running Mechanics and Pelvic Floor Health: The Impact of...
Therapeutic Breast Massage in Lactation (TBML)

Therapeutic Breast Massage in Lactation Can Help Make Breastfeeding Less Painful
Breastfeeding is widely accepted as the normal standard for providing nutrition to newborns, however, many women who do not reach their breastfeeding goals. US national data stated that breast pain was a commonly reported reason for women weaning less than 1 month postpartum. Within that segment, 29% of women who participated in the study stated that “breastfeeding was too painful” to continue.
In the same study, 24% of women reported “breasts feel(ing) too full or engorged” as another reason to discontinue breastfeeding prior to 1 month postpartum.1 Currently, The American Academy of Pediatrics recommends exclusive breastfeeding of infants for the first six months of life. As physical therapists who treat patients with postpartum conditions, we are well positioned to make a big impact on patients with breastfeeding related pain and reduce barriers to continued breastfeeding!
Understanding Relaxin: Why It Doesn’t Cause Pain in Pregnancy

Pregnancy is a time of significant physical and hormonal changes, and among the many hormones involved, Relaxin plays a crucial role. However, there’s a common misconception that Relaxin is responsible for pain during pregnancy. Let’s take a closer look at what Relaxin does and why it doesn’t directly cause pain.
What is Relaxin?
Relaxin is a regulatory hormone involved in growth, metabolism, and tissue remodeling after an injury to our bones, ligaments, muscles or tendons (Dehghan 2014). During pregnancy, Relaxin levels begin to increase in the first trimester to help the body prepare for childbirth by relaxing the ligaments in the pelvis and softening the cervix (Aldabe 2012, Daneau 2014). The ligaments of the pelvis will begin to relax around the 10th-12th week of pregnancy (Aldabe 2012). This process allows for greater flexibility in the pelvic area, facilitating delivery and accommodating the growing baby.
Read more: Understanding Relaxin: Why It Doesn’t Cause Pain in...
- Details
- Written by: Heather Jeffcoat, DPT
- 6555 Views

Optimizing Your Pelvic Floor Health is No Longer a Secret
As pelvic floor physical therapy gains acceptance amongst an ever widening audience, popular websites such as Next Avenue are providing much needed exposure to their readers.
In a recent article entitled "Could Your Symptoms Point to a Pelvic Floor Disorder?", author Brette Sember quotes Heather Jeffcoat as part of this wide ranging discussion of pelvic floor treatments:
Read more: NextAvenue.com | Could Your Symptoms Be Pointing to a...
- Details
- Written by: Staff
- 5865 Views
Believe it or not, the pelvic floor can affect the quality of our breathing.
The opposite is also true:
Promoting efficient diaphragmatic breathing can improve function of the pelvic floor.
In this study by Zivkovic et al. Zivkovic et al. , diaphragmatic breathing exercises were effective in helping to retrain children with voiding dysfunctions, including bowel and bladder issues.
Read more: New Year's Resolutions For Your Pelvic Floor | Breathe!
- Details
- Written by: Staff
- 24632 Views

Don’t squat and hover to pee!
Sit down and relax your pelvic floor muscles.
Ok, ok so this tip is always met with some pushback, but to those of you who prefer to squat and hover to pee rather than sit should be aware that this habit is not good for your pelvic floor! Sit down and relax!
Why is it so bad for you to squat and hover to pee?
When you are in a partial squat, hovering over the toilet, the muscles of your glutes, legs, abs, back, and pelvic floor are activated and cannot fully relax. For urine to flow easily and fully, the pelvic floor muscles and the muscles surrounding your pelvis have to relax.
Read more: New Year’s Resolutions For Your Pelvic Floor | Don't Squat...
- Details
- Written by: Staff
- 14563 Views

Every person with a uterus will experience menopause during their lifetime.
Genitourinary syndrome of menopause (GSM) is a term that describes the different genital, sexual, and urinary signs and symptoms that can occur during menopause.
The symptoms of GSM can greatly affect quality of life, so it is important to be aware the signs so that you can seek out appropriate care and support from your healthcare team.
Read more: What is Genitourinary Syndrome of Menopause (GSM)? And Why...
- Details
- Written by: Staff
- 10810 Views

There Are Several Options For Non-Hormonal Treatments for GSM.
Some include hormones, while others do not.
Today we will review some non-hormone treatment options. As always, consult with your physician to help you make the best decisions regarding your health.
Read more: Management of Genitourinary Syndrome of Menopause |...
- Details
- Written by: Staff
- 15139 Views
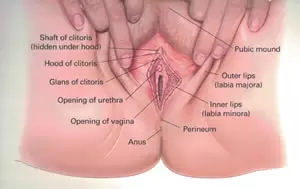
Why Your New Years Resolutions for Your Pelvic Floor Health Should Include Learning Your Anatomy
Have you ever looked at your genitalia in the mirror? Like REALLY looked at it?
One of the most empowering things you can do for your pelvic health is to take a look at yourself in the mirror and learn your anatomy. Here is a quick primer on how to stay on top of what's going on down there, including tips on simple self examination and resources to find more information.
Read more: New Year’s Resolutions For Your Pelvic Floor | Do You Know...
- Details
- Written by: Staff
- 8662 Views

Simple Yoga Poses for Overcoming Foot Pain
Everyone experiences sore feet at some point during our busy lives. Here are a few simple yoga poses that you can do almost anywhere to relieve the pain of sore feet during the busy holiday season - or anytime for that matter!













