What are Kegels?
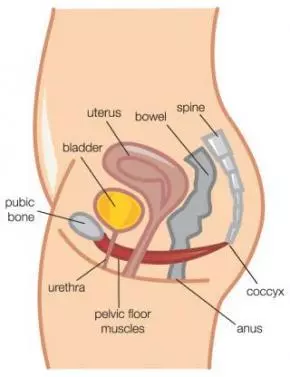
Kegels are a contraction of the pelvic floor muscles, sometimes referred to as “PC Contraction”. PC is short for “pubococcygeus”, the name of one of the many pelvic floor muscles.
However, after over a decade of practice, I have found that simply telling a patient to “Do Kegels” is usually not enough. Often, women perform pelvic floor exercises incorrectly, or do not do an amount appropriate for their strength levels. This finding has been confirmed by Bump et al in an August 1991 article from the American Journal of Obstetrics & Gynecology, “Assessment of Kegel pelvic muscles exercise performance after brief verbal instruction”.
The results of verbal instruction were 60/40 (60% could/40% could not perform a pelvic floor contraction or, Kegel, correctly). This article also stated that a very high percentage of women that were doing Kegels incorrectly were not only doing them wrong, but doing them in such a way that they were actually making their incontinence WORSE. I have seen this initial frustration with many of my own patients over the year, not realizing before they started physical therapy why they were getting worse. I continue to site this study, as despite it’s age, it was really revolutionary in identifying why so many women think Kegels do not work.
How do I know if I am doing Kegels correctly?
Chances are if you have basic stress, urge or mixed incontinence, and see no improvement in your symptoms, you may not be doing your Kegels appropriately. This is not to say that you don’t know how to do a Kegel, but you many not be doing the proper routine based on your strength levels.
How many do I do? How long should I hold them for? There are different types of Kegels?!
This is where physical therapy comes in. Yes, there are different types of Kegels. Some that work better for increasing overall power and others that are designed to improve endurance. There is even a type of Kegel that helps more with controlling and slowing downward forces on the muscle. How many and what type you do depends on your current level of strength and endurance. This can be determined by a trained women's health physical therapist.
In the July 2003 issue of JAMA, an article entitled “Effect of Behavioral Training With or Without Pelvic Floor Electrical Stimulation on Stress Incontinence in Women” discussed the benefits of using biofeedback, perineal electrical stimulation and behavioral training as a package in order to achieve the quickest recovery with better long-term follow-ups.
At Femina Physical Therapy we utilize all 3 techniques to provide our patients with the most comprehensive care available. Treatment of urge and mixed urinary incontinence will include learning how to correctly utilize urge control strategies. We additionally offer a unique pilates-based regimen in the treatment of pelvic floor weakness diagnoses, such as incontinence or pelvic organ prolapse (also referred to as cystocele, urethrocele, urethrocystocele, or rectocele). With some patients, physical therapy has been a welcomed alternative or adjunct to pelvic floor surgery.
Other Women’s Health diagnoses we currently treat include post c-section and hysterectomy adhesion pain; pre-natal/post-partum related musculoskeletal disorders, such as lower back pain, hip pain, SI joint dysfunction, pregnancy-induced carpal tunnel syndrome, diastasis recti, post-partum pelvic pain, other pelvic pain (vaginismus, vulvodynia, vestibulodynia, vulvar vestibulitis, overactive pelvic floor, hypertonic pelvic floor disorder, etc); osteopenia/osteoporosis postural and strengthening programs. We also offer a pilates-based approach to the treatment of general musculoskeletal disorders. All treatment sessions are one-on-one with a licensed physical therapist. Support staff is never used, which keeps the standard of care we provide at the highest level.