Postpartum Stress Urinary Incontinence Affects Many
Motherhood ushers in a lot of changes, both emotionally and physically, for those who take on the role. While it can lead to a new sense of purpose and feelings of unconditional love, it can simultaneously lead to worry, physical exhaustion, and, in the case of multi-hyphenate talent Whitney Port: bladder leakage.
When I started working out after having [my son] Sonny, I experienced bladder leakage trying to do jumping jacks or any kind of cardio," Port tells mbg.
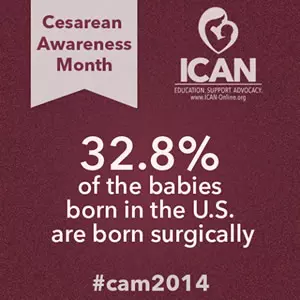
While postpartum stress urinary incontinence may not be one of the joys of having children, it is an incredibly common side effect—both from vaginal and cesarean deliveries.
Mommy Tummy - Not Something You Have to Just Live With

Mommy tummy aka diastasis recti abdominis (DRA) is a prevalent issue.
One in three American moms have DRA that persists greater than a year.
So what is a diastasis recti? It is the stretching of the linea alba, a connective tissue that runs down the midline of the abdomen and connects the abdominal muscles. The stretching happens during pregnancy in almost 100% of mothers to make room for a growing baby. Many of these moms are told this is a normal part of pregnancy, even by their healthcare providers.
DRA is not just about appearance, it is also connected to pelvic floor dysfunctions as well as pelvic and low back pain. In a study by Kari Bo et al., they found that mothers in the US with DRA were also more likely to have the following:
Motherly | Postpartum Exercise Guidelines are Changing

Heather Jeffcoat, DPT
How Postpartum Exercise Guidelines are Changing and Why
We're not saying "Don't exercise at all!"
In the article Sydni describes the evolution of standard practice for exercising postpartum - with recommendations increasing from six weeks to twelve weeks before any strenuous activity - but with added emphasis on easing into exercise at the six week mark, all the while building to a full regimen at the twelve week mark.
She begins:
Many women can’t wait to start exercising again after pregnancy. For others, sweet baby snuggles tend to win out over exercising for the first few weeks. Once you catch up on sleep and start to gain more energy, you may be ready to do Pilates or go for a jog again—but it might not be safe to jump back in with the same intensity level in your postpartum exercise as in your pre-pregnancy routines.
...It turns out, new research backs waiting until 12 weeks postpartum to do high-intensity workouts, and many OBGYNs have adjusted their postpartum exercise recommendations acccordingly.
Motherly | When To Start Exercising Postpartum: New Guidelines Aimed at Protecting Your Pelvic Floor

Heather Jeffcoat
Wondering When To Start Exercising Postpartum? Exercise Guidelines Are Changing
Here’s Why Some Obgyns Recommend Waiting 12 Weeks After Birth To Workout
If you’ve just had a baby, you may be wondering when to start exercising postpartum. There is so much to keep up with when you have a newborn that it's only natural that exercise is often the last thing on your mind right after giving birth.
But once a little bit of a routine has set in, your body will (hopefully) give you some signs that it's time to step it up a bit:
Negotiating Physical Activity for Perinatal Mental Health

Negotiating Physical Activity for Perinatal Mental Health
Exercise is commonly prescribed as one method to help improve one’s mental health (Ekkekakis 2013, Hu et al 2020, Heissel et al., 2023, Stubbs et al 2018, Vella et al 2023). However, a major barrier to begin an exercise routine can often be lack of motivation and fatigue, which is experienced by those suffering from depression (Faulkner and Biddle 2004, Glowacki et al 2017). Postpartum depression and other mental health illness is quite common, with research suggesting a prevalence of up to 20% in new mothers (Bauer et al 2014). Many new moms are told by health care providers to exercise during pregnancy and postpartum. However, advice and guidance on how to overcome barriers to exercising, including mental health barriers, is not addressed often enough.
Most research is focused on the benefits of exercise for mental health support in the general population and postpartum, but rarely addresses the barriers the postpartum population experiences related to mental health. An online survey by Goncalves et al recently set out to fill this gap in knowledge, exploring how women negotiate physical activity for their mental health and the barriers to participating in physical activity associated with mental health illness. 186 mothers were included in the study, from 6 weeks postpartum up until 4 years postpartum, three main themes were found in this qualitative study: barriers to physical activity associated with mental illness, strategies to negotiate being active for perinatal mental health, and guilt associated with not being active enough.
NormaTec Therapy

We are excited to announce the addition of the NormaTec PULSE Series to our treatment options!
NormaTec is the ultimate recovery device. The technology can increase circulation and improve mobility for those who work out regularly, are training for a competition or race, experience swollen legs from traveling frequently, stand for long hours on the job, or suffer from inflammation, sore muscles, or other circulatory issues.
NormaTec is used extensively in professional athletics and is utilized for both rehab and recovery by 97% of pro teams, as well as Olympic and elite athletes across a broad spectrum of sports. Plus, our pregnant and post-operative patients love the way they feel after a session!
Pelvic Floor Injury During Childbirth: All About Levator Ani Avulsion

Levator Ani Avulsion: Understand your pelvic anatomy to better understand your injury
The pelvic floor is a group of muscles positioned like a hammock along our saddle region.
The group of muscles attach from our pubic bone on the inside and then to our lateral pelvic walls with a bundle of collagen fibers called the levator arch, and attach to the ischial spines (the inside of the sit bones) and tailbone on the back side. During vaginal childbirth, the pubococcygeus muscle, a group of pelvic floor muscles, stretches 3.26 times more than its normal length to make room for the coming baby in the vaginal canal! As you can imagine, this may result in some perineal tearing and/or levator ani avulsion.
Pelvic Floor Physical Therapy after Cesarean Section

What Pelvic Floor Physical Therapy after Cesarean Section Can Do For You
Physical therapy after cesarean section can help you in your recovery by giving you skills to regain optimal body function and help you get back on your feet, doing the activities you value in addition to taking care of your new little one. In this article we review some ways that a therapist at Femina Physical Therapy can help you through your recovery. You can see a trained therapist as soon as you have the energy to do so.
Scar management and desensitization
Pelvic floor physical therapists are trained in soft tissue mobilization techniques to help soften and flatten scar tissue after your cesarean incision is healed. As a part of your treatment, your therapist will teach you techniques such as scar massage to help prevent scar tissue build up and puckering. Check out our full article on scar tissue management here.
POP Quiz About Two Common Postpartum Conditions - Pelvic Organ Prolapse and Urinary Incontinence

What are Pelvic Organ Prolapse and Urinary Incontinence?
What is the biggest risk factor for both conditions? And how can you tell if you have them?
Not sure? You’re not alone. In fact, one research study found women actually know more about erectile dysfunction than they do about pelvic organ prolapse! While pharmaceutical company advertising bias may be to blame for part of that equation, one of the largest surveys of pregnant women and new moms ever conducted on the subject (by a team of medical experts in New England) reveals women’s healthcare providers consistently miss their biggest window of opportunity to educate patients about these conditions and offer treatment strategies that work.
Post-Partum Renewal Program

Our Premier Post-partum physical therapy program in Los Angeles is a complete evaluation for diastasis rectus abdominus, postural and movement dysfunctions and pelvic floor muscle status. Treatments may include pelvic floor muscle biofeedback, specific strengthening exercises and an educational program, manual therapy to address myofascial restrictions -- all custom-tailored with your specific goals in mind. Our goals are to help you get back to all of the activities you were doing before baby.
Postpartum Anal Incontinence

What is Anal Incontinence?
Anal Incontinence is defined as the complaint of involuntary loss of liquid or solid stool or the involuntary loss of gas.
It is supposedly an underreported condition because of its stigmatizing nature. It occurs in approximately 50% of women at long-term follow-up after anal sphincter injuries (Gommesen et al., 2019; Haylen et al., 2010; Damon et al., 2006; Cotterill, 2008).
Postpartum Leggings for Support and Comfort After Birth

Comfort After Birth is Possible With Postpartum Leggings
Heather Jeffcoat, DPT
Bringing a new life into the world is a transformative chapter where a woman's body undergoes profound changes.
Maternity leggings provide comfort to one's growing bump, but postpartum leggings? They're like a full-body hug, providing the indispensable support and comfort your body craves as it gracefully heals.
In a recent interview with The Bump, I emphasized that:
Postpartum Pelvic Pain and What You Can Do About It

Pelvic pain during the postpartum period is common, even for those who had a “perfect and easy” pregnancy, labor and delivery. Often times, healthcare providers will tell women that the pain “will get better with time,” however it's important to advocate for yourself and seek out care if you feel like you need it. Read my previous article about advocating for your postpartum care here.
Common types of postpartum pelvic pain and what you can do at home:
Vaginal Dryness
After delivery, your estrogen levels drop and progesterone levels stay high, especially if your are breastfeeding.
What you can do:
A simple solution can be drinking more water and using a water-based lubricant, read my previous blog on choosing the right lubricant for you.
Postpartum Sexuality & Mood Changes in Women with Pelvic Girdle Pain

Does my pelvic girdle pain have anything to do with my mood and sexuality?
Many of our patients experience sexual dysfunctionandanxiety, depression and chronic pain. These conditions are known to coexist, and we unpack each component of pain, mood and one’s behaviors, desires and attitudes related to sex and physical intimacy.
Pelvic girdle pain isdefined as “pain between the posterior iliac crests and gluteal folds particularly in the vicinity of the sacroiliac joint” (Simonds). More simply stated: in the very low area of your back and buttock. Pelvic girdle pain is common postpartum and may impact disability in the fourth trimester. Many are aware of peripartum symptoms such as low back pain, incontinence,pelvic organ prolapse, pain with intercourse, and postpartum depression. Knowing that many women experience pain during and after pregnancy - what can we learn about the effects of pelvic girdle pain? Specifically, what impact does pelvic girdle pain have on symptoms of mood and sexuality?
Pregnancy & Postpartum Issues - Pain, Dysfunction and Fitness

Pain, Dysfunction, and Other Pregnancy & Postpartum Issues
We can help with a large range of pregnancy and post-partum related disorders. We also offer a post-hysterectomy recovery program and many other pregnancy and non-pregnancy related services.
Redefining Postpartum Care in the “Fourth Trimester”

Redefining Postpartum Care in the “Fourth Trimester” by Utilizing Pelvic Floor Physical Therapy
Last month the American College of Obstetricians and Gynecologists (ACOG) updated their position on postpartum care in the “fourth trimester” - the first 12 weeks after your baby is born. This is such a huge step for better healthcare and support for women after delivery. In other countries (France, Belgium, Northern Ireland and other European countries), postpartum physical therapy is a routine referral for women both in the hospital and for ongoing support when they are discharged.
The statement updates the previous recommendation of a 6 week visit, and instead supports a paradigm shift of postpartum care that not only adds contact with their Ob-Gyns within the first 3 weeks of delivery, but also address the need for ongoing care:
Restless Legs Syndrome & Physical Therapy | Postpartum Recovery Series - Part 3

Restless Legs Syndrome (or RLS)
Restless legs syndrome (or RLS) is a condition where there are uncontrollable urges to move limbs (mostly in the legs, but sometimes in the arms) that follows a circadian pattern, namely evenings/overnight when resting.
The urges usually come with unpleasant sensations such as tingling, burning, itching, or otherwise pain. Usually, it can be alleviated by movement, but as you can imagine, it can be debilitating and impair sleep, and thus the quality of life. It is common to experience mood swings, anxiety, and depression.
It is estimated that about 3.9-14.3% of the general population suffers from RLS. It is the most common movement disorder in pregnant women. There is either primary (idiopathic) RLS, or secondary (acquired) RLS due to pregnancy, renal pathologies, diabetes, hypertension, and other metabolic conditions. The two most common risk factors for RLS are iron deficiency and kidney disease.
Safely Returning to Activity and Sport | Postpartum Recovery Series - Part 1

Safely Returning to Activity and Sport Postpartum
Postpartum Recovery Part 1
Most women get the clearance after their 6 week check-up for sex and exercise, YAY! But, really? How? What does that mean? There are no guidelines on how to return to activity in a safe, leak-free and pain-free manner.
Between 6 and 31% of postpartum women experience urinary incontinence. In addition, 66% of those who experience urinary incontinence during pregnancy and/or their first 3 months of postpartum continued to experience incontinence even at 12 years after birth! As you can see, it may be common, but it is certainly not normal!
Scar Management and Desensitization After C-Section, Hysterectomy, and Laparoscopic Procedures
Tips For Scar Management and Desensitization After C-Section
Also After Hysterectomy and Other Laparoscopic Procedures
After delivery via cesarean section, hysterectomy or other laparoscopic procedure, there will be an incision site that you will have to manage according to the directions of your doctors and nurses to keep the site from becoming infected. Although the incision site will close after about 2-3 weeks, scar tissue will continue to form. It is important to begin scar massage and desensitization techniques to help prevent scar tissue build up, puckering, and ongoing pain.
Managing Scar Tissue
A trained physical therapist can perform soft tissue mobilization and other modalities such as cold laser over the scar site. As a part of your treatment, your therapist will teach you skills to manage the scars at home for the following benefits:
Sex After Childbirth – What’s Your ‘New Normal’?

You counted down the weeks until your baby’s arrival…
now you and your partner are counting down the days until your doctor gives you the green light to have sex again.
That’s a good thing; intimacy is an important factor in your relationship and your own well-being. But whether this is your first baby, or you’re sure it’s your last, your anticipation might be tinged with some anxiety. After all, your body has been through a lot since that positive pregnancy test result.
Sleepless nights, fluctuating hormones, and breastfeeding challenges can take a toll. Perhaps you’re still healing from a C-section or a physically challenging delivery. Even if giving birth was a breeze, and this is your easiest baby yet, you may worry that your expectations aren’t in sync with your partner’s.
When it comes to your postpartum sex life, what’s the new normal? And how soon can you get there?
Testimonial by Y.L. (mom of 2)
After having my second baby via C-section I searched for months to try to find help for my lower back pain and separated abdominal muscles. I finally came across Heather Jeffcoat via a mommy blog. I reached out to her via email and set my first appointment. My first appointment went amazing … she listened to what my symptoms, check my separation and explained to me in detail what the next steps would be. Not only did my abdominal separation go from 3 to about 1 -1/2 but my back has pain has significantly reduced. I’m personally recommending all my mommy friends to Heather!
The Effects of Pelvic Floor Muscle Strength on Orgasm

Let's Look at the Effects of Pelvic Floor Muscle Strength on Orgasm
Hint: strong pelvic floor muscles = strong orgasm
The world is learning more and more about the pelvic floor and the many ways that it can be treated. At Femina Physical Therapy, we have spoken about pelvic rehab for urinary, bowel, birth, pregnancy, bladder, erectile issues, and many more. But we all know the question that everyone wants answered: Does pelvic floor strength affect orgasm?
Well reader, you came to the right place.
Therapeutic Breast Massage in Lactation (TBML)

Therapeutic Breast Massage in Lactation Can Help Make Breastfeeding Less Painful
Breastfeeding is widely accepted as the normal standard for providing nutrition to newborns, however, many women who do not reach their breastfeeding goals. US national data stated that breast pain was a commonly reported reason for women weaning less than 1 month postpartum. Within that segment, 29% of women who participated in the study stated that “breastfeeding was too painful” to continue.
In the same study, 24% of women reported “breasts feel(ing) too full or engorged” as another reason to discontinue breastfeeding prior to 1 month postpartum.1 Currently, The American Academy of Pediatrics recommends exclusive breastfeeding of infants for the first six months of life. As physical therapists who treat patients with postpartum conditions, we are well positioned to make a big impact on patients with breastfeeding related pain and reduce barriers to continued breastfeeding!
Vaginal Childbirth Positioning Series | Part 3: Delivery of the Placenta

Third Stage of Childbirth: Delivery of the Placenta
You made it!
Now, at this point you have delivered your baby and your body’s hormones have shifted tremendously! You may feel overwhelming emotions of joy and exhaustion at the same time. Oxytocin, the bonding hormone, rises sharply to compensate for the drastic drop in estrogen and progesterone. You may find yourself shivering, and this is normal immediately post-giving birth and can last up to one hour.
Delivery of the Placenta
Verywell Family | 5 Best Diastasis Recti Exercises

If you’re looking for specific diastasis recti exercises, we can help you get back into a fitness groove after pregnancy and childbirth and help heal and strengthen the deep core muscles.
What is Diastasis Recti?
Diastasis recti happens when the two muscle bellies of the rectus abdominis separate. The separation between the right and left sides of this muscle can happen during pregnancy when the linea alba, or the tissue between the rectus abdominis muscles, stretches to allow the body room for your baby.
Your OB/GYN or physical therapist can determine if the separation you have is considered wide enough to be diastasis recti. In general, separation of more than two centimeters at one or more points of the linea alba meets the criteria for diastasis recti.1
Visually, diastasis recti can look like a bulge of the abdominal contents or a pooch in your belly area. Physically, you may notice back pain, abdominal weakness, and poor posture.
Verywell Family | How Long After Pregnancy Can You Have Sex?

Wondering How Long After Pregnancy Can You Have Sex?
Your world changes drastically after having a baby. Feeling in the mood for sex may take some time for both you and your partner. And whether you’re dealing with a lack of sleep, hormonal ups and downs, painful recovery, postpartum depression, trouble connecting with your partner, or all of the above, trying to rush an intimate relationship can cause more trouble than its worth.
That’s why it’s important to ease back into this part of your life and educate yourself on what to expect. Here, we go over the recommended wait time, reasons why you might be experiencing painful sex, why it’s normal to not want to have sex right away, and tips for when you are ready.
What do Breastfeeding Women Need and Want? - No One Told Me About This Part!

What do Breastfeeding women need and want? Let's take a closer look.
You’ve had your bundle of joy and you’re working out the kinks of having a new baby in your life and feeding them the best you can. From breastfeeding to return to exercise, there are many challenges that new moms must navigate.
There are a wide range of feeding options, from exclusively breastfeeding to formula/food feeding or a combination of the two. Studies have tried to get a better understanding of what women need in this stage of motherhood, particularly determining what impacts breastfeeding may have on exercise and activity. We know that breastfeeding causes a depression in estrogen which in turn can cause pelvic floor dysfunction like the involuntary leakage of urine with activities such as sneezing, coughing, laughing or exercise defined as stress urinary incontinence. This type of incontinence has been linked to a longer duration of breastfeeding, however its effects are not lasting (Snyder). Breastfeeding people may also have breast-related discomforts such as nipple pain, mastitis, and over/under supply. Any of these symptoms may limit one’s motivation to exercise.