Every person with a uterus will experience menopause during their lifetime.
Genitourinary syndrome of menopause (GSM) is a term that describes the different genital, sexual, and urinary signs and symptoms that can occur during menopause.
The symptoms of GSM can greatly affect quality of life, so it is important to be aware the signs so that you can seek out appropriate care and support from your healthcare team.
What is Menopause?
Every person with a uterus will experience menopause during their lifetime and it is a normal part of aging. Menopause marks the end of a woman’s reproductive years. It typically happens naturally in a woman’s late 40s to early 50s, but it can also be triggered by surgical removal of the ovaries.
What is GSM?
Genitourinary syndrome of menopause (GSM) is a relatively new term that describes the different genital, sexual, and urinary signs and symptoms that can occur during menopause.
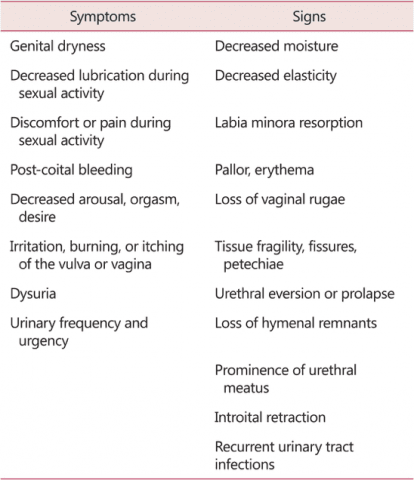
Here is a table that outlines the different signs and symptoms of GSM, originally printed in Portman, 2014:
Why should you know about GSM?
Every person with a uterus will experience menopause during their lifetime, and the symptoms of GSM can greatly affect quality of life. Therefor it is important to be aware the signs so that you can seek out appropriate care and support from your healthcare team.
Genital Symptoms
Genital symptoms including vaginal dryness can affect your sex life and general comfort. These symptoms include vaginal dryness, pain with penetration (dyspareunia), vaginal irritation, genital itching, vaginal tenderness, and vaginal bleeding or spotting during intercourse. According to a study by Nappi et al. (2010), between 45% to 63% of postmenopausal women have these symptoms, so it is quite common. It is also apparent that these symptoms negatively affect satisfaction with sex; according to Levine et al. (2008), sexually active postmenopausal women with sexual dysfunction are four times more likely to genital symptoms than those without sexual dysfunction.
These symptoms relate to the reduction of estrogen circulating in the blood. The tissues of the vagina, vulva, pelvic floor muscles, urethra, and bladder respond to estrogen levels. When there is less available estrogen in the system, the tissues of these areas can thin, have less elasticity, and become more vulnerable to irritation and damage.
Urinary Tract Symptoms
Estrogen deficiency after menopause can cause lower urinary tract symptoms, including painful or difficult urination (dysuria), urgency, frequency, increased night time urination (nocturia), urinary incontinence (UI), and recurrent UTI (Robinson, 2003).
In one study by Robinson (2003), 20% of postmenopausal women reported urinary urgency and almost 50% had stress urinary incontinence (SUI). Again, estrogen deficiency seems to affect the health and function of the tissues and muscles of the urinary tract, including the bladder, urethra, and associated tissues.
Do you have GSM? What you can do.
Go see your doctor. The most important thing for you to do is be under the regular care of a doctor. Gynecologists and women’s health nurse practitioners can be a great resource as you transition to menopause. Your doctor will also be able to discuss treatment options with you, including hormone therapy, non-hormonal treatment options, and also give you a referral to pelvic floor therapy.
Contact a pelvic floor therapist. Pelvic floor therapy can help with common menopausal pelvic health issues including urinary incontinence, bowel issues, pain with sex, and pelvic pain. Check out our past blog post on Menopause and Pelvic Health.
References
Kim, H. K., Kang, S. Y., Chung, Y. J., Kim, J. H., & Kim, M. R. (2015). The Recent Review of the Genitourinary Syndrome of Menopause. Journal of menopausal medicine, 21(2), 65–71. doi:10.6118/jmm.2015.21.2.65
Portman DJ, Gass ML. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21:1063–1068. [PubMed] [Google Scholar]
Nappi RE, Kokot-Kierepa M. Women’s voices in the menopause: results from an international survey on vaginal atrophy. Maturitas. 2010;67:233–238. [PubMed] [Google Scholar]
Levine KB, Williams RE, Hartmann KE. Vulvovaginal atrophy is strongly associated with female sexual dysfunction among sexually active postmenopausal women. Menopause. 2008;15:661–666. [PubMed] [Google Scholar]
Robinson D, Cardozo LD. The role of estrogens in female lower urinary tract dysfunction. Urology. 2003;62:45–51. [PubMed] [Google Scholar]
Callan, N. G. L., Mitchell, E. S., Heitkemper, M. M., & Woods, N. F. (2018). Constipation and diarrhea during the menopause transition and early postmenopause. Menopause, 25(6), 615–624. doi:10.1097/gme.0000000000001057
Castellani, D., Saldutto, P., Galica, V., Pace, G., Biferi, D., Paradiso Galatioto, G., & Vicentini, C. (2015). Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence. Urologia Internationalis, 95(4), 417–421. doi:10.1159/000381989
Maltais ML, Desroches J, Dionne IJ. Changes in muscle mass and strength after menopause. J Musculoskelet Neuronal Interact. 2009;9(4):186-97
Minkin, M. J., Reiter, S., & Maamari, R. (2015). Prevalence of postmenopausal symptoms in North America and Europe. Menopause, 22(11), 1231–1238. doi:10.1097/gme.0000000000000464
Mehta, R. S., & Staller, K. (2018). Menopausal transition and bowel disturbances. Menopause, 25(6), 589–590. doi:10.1097/gme.0000000000001110

