When it Comes to Sex With a Hip Impingement, Position Really Does Matter
It's no surprise that if you recently had hip surgery - or have an ongoing hip issue - that your sex life could suffer. Read on for some recommendations.
What is Femoroacetabular Impingement (FAI) Syndrome?
Femoroacetabular impingement (FAI) syndrome is a disorder of the hip that typically affects young adults. It is the result of an abnormal contact between the greater trochanter of the femur (thigh bone) and the acetabulum (the socket).
FAI is one of the most common reasons why people undergo arthroscopic surgery on their hips, but many people are treated via conservative pathways (PT, rehabilitative exercise, joint injections). The symptoms of FAI syndrome include motion- or position-related hip and/or groin pain. Pain may also be felt in the back, buttock or thigh. In addition to pain, patients may also describe clicking, catching, locking, stiffness, restricted range of motion or giving way. (Griffin et al., 2016).
Hip Issues Affect Your Sex Life
It makes logical sense that having FAI and other ongoing hip issues could put a damper on your sex life. Sex can require a lot of interesting positions and hip motions, which are not always egonomic. Researchers Lee et al. (2015) confirmed this hypothesis when they found that most patients with femoral acetabular impingement syndrome (FAI) reported sex with a hip impingement to be difficult due to their discomfort.
A new study by Morehouse et al. (2020) used state of the art imaging techniques to see the kind of stress 15 different sex positions put on your hip joint. FYI the definition of sex for this study was penetrative sex between a heterosexual couple… However I think we can extrapolate findings for those engaging in non-heteronormative play!
The aim of the study was to identify positions for sex with a hip impingement that could be recommended to patients who had recently undergone hip arthroscopy, or who had ongoing hip impingement issues or were at risk for developing a hip impingement issue.
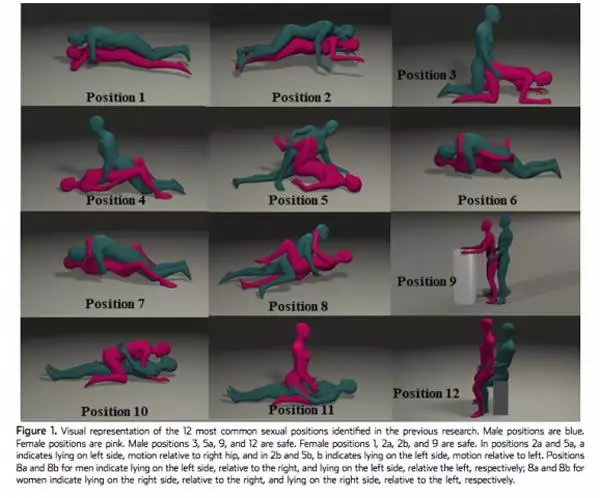
12 common sexual positions were reviewed via MRI to see the kind of hip motion that is required of both participants, and the study identified positions that are either safer or less safe for those who have had recent hip surgery or ongoing impingement.
You can see these positions in this diagram (click/tap to see full size):
Image from Morehouse, H., Sochacki, K. R., Nho, S. J., & Harris, J. D. (2020). Gender-Specific Sexual Activity After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: Position Matters. The Journal of Sexual Medicine. doi:10.1016/j.jsxm.2019.12.026
Safe Movement Paramaters
Hips get more unstable with more than 0 degrees of hip extension (think leg going out behind you), greater than 30 degrees of external rotation (think knees pointing “out” or duck feet), or greater than 30 degrees of abduction (think “spread eagle”). Hips face a larger risk of impingement if the hips go past 90 degrees of flexion (knee to chest), more than 10 degrees of internal rotation (going “pigeon toed”), and more than 10 degrees of adduction (legs crossing midline). Perhaps a little confusing for those of you who have not taken anatomy classes, but bear with me!
Using these recommendations listed above, if the “blue character” is the person with hip issues, the safest positions are 3, 5 (when laying on the problem side), 9, and 12.
If the “pink character” is the person with hip issues, positions 1, 2 (laying slightly on left or slightly on right side), and 9 are safest.
You’ll notice that the safe positons for sex with a hip impingement stay in line with the safe movement recommendations listed above: legs don’t tend to go back behind you, knees and legs stay neutral (no turning in or out), and hips don’t go into too much flexion (knee to chest), avoid too much abduction (spread eagle), and also avoid any crossing of the legs past midline.
Recommendations for Those Who Have Had Recent Hip Surgery
Current evidence shows 100% capsular healing at 24 weeks post-op, so if you’ve had hip surgery recently, you should be safe to have sex after 6 months. Keep in mind this is a conservative recommendation, because some wonder-kids are pain free 48 hours after operation. So, if you feel comfortable talking with your doctor about this, ask them for their opinion.
If you are confused by all of the anatomical terms of this blog post and in the journal articles, come see one of our therapists and we can give you some personalized recommendations, based on our in depth evaluations and treatment sessions. Give us a call or make an appointment today!
References
Griffin DR, Dickenson EJ, O’donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016;50:1169-1176.
Morehouse, H., Sochacki, K. R., Nho, S. J., & Harris, J. D. (2020). Gender-Specific Sexual Activity After Hip Arthroscopy for Femoroacetabular Impingement Syndrome: Position Matters. The Journal of Sexual Medicine. doi:10.1016/j.jsxm.2019.12.026
Lee S, Frank RM, Harris J, et al. Evaluation of Sexual Function Before and After Hip Arthroscopic Surgery for Symptomatic Femoroacetabular Impingement. Am J Sports Med 2015; 43:1850-1856.