Learn How Obesity Increases Urinary Incontinence and How Pelvic Floor Therapy Can Help
Urinary Incontinence is common, why suffer?
Urinary incontinence is the loss of bladder control. Urinary incontinence affects up to 1 in 3 women. The two most common types of urinary incontinence that affect women are stress incontinence and urge incontinence (also called overactive bladder, or OAB). Incontinence affects twice as many women as men. This may be because pregnancy, childbirth, and menopause are contributing factors to urinary incontinence. Urinary incontinence should not be considered a normal part of aging, and it can be treated.
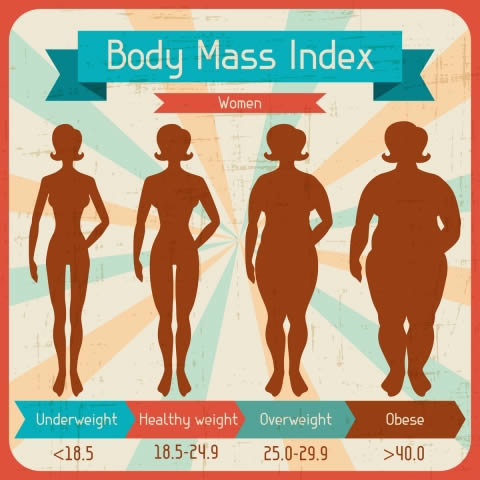
A new article published in September, 2018 by Lamerton, Torquati, & Brown found that being overweight (BMI 25-30) increased risk of urinary incontinence for young and middle aged by 35% and obesity (BMI ≥30) almost doubles the risk at 95%.
The findings of this study are important because those with urinary incontinence when young and middle aged adults are more likely to have worse symptoms when they are older. Another reason why the study is important is that weight, relative to factors like genetics, is a risk factor that can be controlled with diet and exercise.
What is urinary incontinence?
Urinary incontinence refers to the loss of urine, out of your control. There is actually more than one kind of urinary incontinence:
- Stress Incontinence: leaking with activities like coughing, sneezing and jumping
- Urge Incontinence: leakage associated with urgency: waiting for the restroom, putting the key in the door, fumbling with your pants, etc.
- Mixed UI – a combination of stress and urge symptoms
How does weight affect urinary continence?
The findings of this study suggests that excess abdominal weight places increased pressure on the bladder and pelvic floor muscles. When the pelvic floor muscles have increased demand on them (holding your organs up), they can get weak, which can lead to urinary leakage.
What you can do to Prevent Urinary Incontinence
There are lots of factors besides weight that contribute to urinary incontinence. If you have any concerns regarding your pelvic health, it is always best to get a thorough evaluation from your doctors and a pelvic floor therapist (licensed physical therapist that specializes in pelvic health).
Here is a short list of things that can contribute to urinary incontinence:
- Ingesting a lot of bladder irritants (alcohol, coffee, soda, citrus, tomatoes, chocolate, carbonated drinks, among others).
- Drinking too much water, or not enough water. Chugging a quart of water in one sitting may overwhelm your bladder and create a strong sense of urgency. However, not drinking enough water will cause your urine to be too concentrated, which will irritate the bladder and contribute to leakage. Golden rule of thumb is to drink 64 oz of water a day (or more if it is hot or humid out, or your activity demands increase) and drink smaller amounts of water at a time. Try sipping throughout the day from a water bottle, or having a half glass of water every hour.
- Medications including blood pressure drugs, heart medications, diuretics, muscle relaxants, antihistamines, sedatives and antidepressants can contribute to incontinence. If you are taking these medicines and develop issues with urination, see your doctor.
- Weight. As we’ve been discussing in this article, excessive body weight can add pressure on your bladder and pelvic floor, resulting in leakage. Maintaining a healthy weight with activities, diet, and exercise may help with leakage.
- Smoking. The nicotine in tobacco has been shown to irritate the muscle that controls the bladder (Wyman, Burgio, & Newman, 2009). Smokers are also likely to have a chronic cough which can create more pressure on the bladder and pelvic floor.
- Constipation. As we’ve written about in the past, straining with bowel movements can damage the pelvic floor. Exercising, drinking enough water and eating high-fiber foods, such as lentils, beans, and fresh vegetables and fruit, might help improve constipation.
- Weak pelvic floor muscles. Weakness in the pelvic floor can be due to the muscles being too tight or too weak and underactive. A pelvic floor therapist can help determine what is going on with your pelvic floor.
How Pelvic Floor Therapy Can Help
If you have urinary leakage, make an appointment with a pelvic floor therapist. Pelvic floor therapy can help figure out what overlapping issues are contributing to your urinary incontinence.
What does pelvic floor therapy look like?
The treatment modalities you will receive in pelvic floor therapy depend on your body and the issues present.
Some of the modalities used at Femina Physical Therapy for the treatment of urinary incontinence can include (but are not limited to):
- Bladder and bowel habits including lifestyle modifications like optimal fluid intake and constipation management
- Therapeutic exercise to strengthen the pelvic floor
- Biofeedback training with intravaginal sensors
- Electrical stimulation using the InTone device
- Manual therapy to treat connective tissue dysfunction and myofascial trigger points
- Visceral mobilization (gentle massage techniques that loosen internal adhesions and restore movement to the organs including the intestine, bladder, uterus, and ovaries) to reduce intra-abdominal pressure, improve motility, and organ function
- Internal pelvic manual therapy to treat sensitive tissues, muscle spasms, trigger points, and muscle guarding that can contribute to urgency, frequency, and leakage
- Training in self treatment techniques including correct form for pelvic floor strengthening and abdominal lymphatic massage
- Neuromuscular re-education and autogenic relaxation to reduce chronic muscle over-activity and improve parasympathetic nervous system function, including reducing bladder spasms
Contact one of our Los Angeles area offices for more information. November is Bladder Health Awareness month and we will be posting articles all month on this important topic, so check back often or better yet join our mailing list so you don't miss out!
Resources
Lamerton, T. J., Torquati, L., & Brown, W. J. (2018). Overweight and obesity as major, modifiable risk factors for urinary incontinence in young to mid-aged women: a systematic review and meta-analysis. Obesity Reviews. doi:10.1111/obr.12756
Mayo Clinic. Bladder control: Lifestyle strategies ease problems. . Accessed 10/15/18 at https://www.mayoclinic.org/diseases-conditions/urinary-incontinence/in-depth/bladder-control-problem/art-20046597
Wyman, J. F., Burgio, K. L., & Newman, D. K. (2009). Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence. International Journal of Clinical Practice, 63(8), 1177–1191. doi:10.1111/j.1742-1241.2009.02078.x