There Are Several Options For Non-Hormonal Treatments for GSM.
Some include hormones, while others do not.
Today we will review some non-hormone treatment options. As always, consult with your physician to help you make the best decisions regarding your health.
Review: What is GSM?
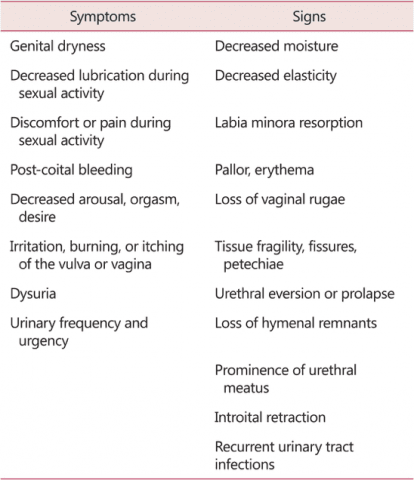
As we discussed in a previous post, genitourinary syndrome of menopause (GSM) is a relatively new term that describes the different genital, sexual, and urinary signs and symptoms that can occur during menopause.
Here is a table that outlines the different signs and symptoms of GSM, originally printed in Portman, 2014:
Non-Hormonal Treatments of GSM
Use it or Lose it: Maintain Sexual Activity
Maintaining some regularity in your sexual activity, including partnered sex or masturbation, will stimulate vaginal, vulvar, and genital tissues and help maintain sexual function. Use of dilators, vibrators, and penetrative sex will stimulate and stretch the vulvar and vaginal tissues to maintain function. Sexual arousal will increase circulation to the genital tissues, and orgasm will help circulate blood and lymphatic fluid out of the pelvic bowl also.
Lubricants and Moisturizers
Lubricants can be used as needed for sexual activity to increase comfort and pleasure. Check out our prior blog post on lubes to help you choose a lube that won’t damage your tissues.
Lube can:
- Be used for penetrative and non-penetrative sex, masturbation, and sex toy play
- Improve lubrication, pleasure, and moisture
- Decrease friction and discomfort
- Decrease failure of sexual barriers (IF COMPATIBLE, more on that later)
- Takes some pressure off the body to “perform” and create enough moisture
- Makes sexual activities possible for many folks
Common types of lubricants: oil, water-based, and silicone
Water-based lubes
Ideal for people with sensitive skin or vaginal irritation and are safe to use with condoms and sex toys. However make sure your lube has proper osmolality and pH level (read below). Water-based lubes tend to get “sticky” and you may need to re-apply if you are engaging in sex for a long time.
Silicone-based lube
Very slippery and long lasting and is safe to use with condoms. However, silicone-based lubes cannot be used with silicone sex toys, as they can damage the toy. Silicone-based lubes may be more difficult to wash off skin than water-based and may stain sheets, so keep that in mind.
Oil-based lube
We like to recommend organic coconut oil. Oil based lubes are slippery and last longer than water-based lubes. However, oil based lubes are not compatible with latex condoms, as they make the condoms easier to break. Like silicone-based lube, oil-based can stain sheets and be harder to wash off than water-based lube.
Vaginal Moisturizers
Long-term vaginal moisturizers are designed to be used daily or every few days on a regular basis to maintain vulvar and vaginal moisture. These moisturizers are designed to mimic normal vaginal secretions. Read our blog on the importance of picking the right pH and osmolality of lubricants and moisturizers to make sure your lube/moisturizer is not damaging your tissues.
Check out this chart published by the World Health Organization (WHO) listing brand names of lubricants and moisturizers and the pH levels and osmolalities of each product.
Topical lidocaine
Consult with your doctor to see if a genital-safe lidocaine gel or ointment could help with your pain with sex. Lidocaine temporarily numbs whatever it comes in contact, so it may help reduce pain at the opening of the vagina. However, be aware that lidocaine may affect the sensation of your partner as well.
Pelvic Floor Therapy
Pelvic floor therapy can help with common menopausal pelvic health issues including urinary incontinence, bowel issues, pain with sex, and pelvic pain.
Urinary Incontinence
Losing urine when with coughing, sneezing, and laughing is known as stress urinary incontinence. It is common to hear stories about this, as well as “overactive bladders” and “nervous bladders” which lose urine on the way to the bathroom and with strong urge.
Between 12.8 to 46% of women deal with urinary incontinence during their lifetime, with an increase during and after menopause. This is due to: a reduction of elasticity in the genital tissues, thinning in the tissues lining the urethra (the tube that empties urine from the bladder, and reduced muscular strength in the pelvic floor, the group of muscles that supports your pelvis and keeps your “holes” closed.
How Pelvic Floor Therapy Can Help with Urinary Incontinence
Pelvic floor therapy can help you train your pelvic floor muscles, increasing the strength of the muscles. A pelvic floor therapist can will also correct muscle incoordination that can lead to leakage.
Bowel Issues
The research is inconclusive as to whether or not menopause directly causes or worsens constipation, diarrhea, and Irritable Bowl Syndrome (IBS). However it is clear that stress tension, and anxiety all affect bowel health and regularity.
How Pelvic Floor Therapy Can Help with Bowel Issues
A pelvic health therapist can help you with neuromuscular re-education, biofeedback, and self care techniques such as abdominal massage that can regulate the GI system and promote regularity.
Pelvic Pain and Painful Sex
According to Minkin et al. 77% of women with menopause report vaginal dryness, and about 40% report pain with sexual intercourse and touch to the genitals.
When sex is painful, this can trigger anxiety about sex. This anxiety then triggers a new cycle of sexual problems: muscle guarding, decreased lubrication, and pelvic floor tension.
How Pelvic Floor Therapy Can Help with Pelvic Pain and Painful Sex
A pelvic floor therapist can help break the muscle tension cycle with manual therapy and teaching you self-treatment to maintain gains at home. By releasing pelvic floor tension, you free pelvic floor muscles, allowing for pain free sex. Pelvic floor therapists can also screen for musculoskeletal dysfunction in the spine, hips and pelvis; educate about sexual ergonomics and help you find positions that reduce pain during intercourse. Pelvic floor therapists can also provide you with self care programs which can reduce dryness and irritation in the tissues of the vulva, labia, and vaginal canal.
Photobiomodulation
This year, there has been some research published by Lanzafame et al. showing that photobiomodulation, a type of light therapy using light-emitting diodes (LEDs) or supraluminous diodes (SLDs) with red and near-infrared radiation (NIR) light can be effective in the treatment of vaginal tissue laxity.
The research suggests that PBMT stimulates collagen and elastin production in the vaginal tissue and supporting urethrovaginal sphincter and urethra, which may help with symptoms of GSM. At Femina PT, we have several light therapy machines that can be used for photobiomodulation therapy.
Give the therapists at Femina Physical Therapy a call today!
References
Kim, H. K., Kang, S. Y., Chung, Y. J., Kim, J. H., & Kim, M. R. (2015). The Recent Review of the Genitourinary Syndrome of Menopause. Journal of menopausal medicine, 21(2), 65–71. doi:10.6118/jmm.2015.21.2.65
Portman DJ, Gass ML. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21:1063–1068. [PubMed] [Google Scholar]
Faubion, Stephanie S. et al. (2017). Genitourinary Syndrome of Menopause: Management Strategies for the Clinician. Mayo Clinic Proceedings, Volume 92, Issue 12, 1842 – 1849. Accessed from https://www.mayoclinicproceedings.org/article/S0025-6196(17)30639-0/fulltext
Nappi RE, Kokot-Kierepa M. Women’s voices in the menopause: results from an international survey on vaginal atrophy. Maturitas. 2010;67:233–238. [PubMed] [Google Scholar]
Levine KB, Williams RE, Hartmann KE. Vulvovaginal atrophy is strongly associated with female sexual dysfunction among sexually active postmenopausal women. Menopause. 2008;15:661–666. [PubMed] [Google Scholar]
Robinson D, Cardozo LD. The role of estrogens in female lower urinary tract dysfunction. Urology. 2003;62:45–51. [PubMed] [Google Scholar]
Callan, N. G. L., Mitchell, E. S., Heitkemper, M. M., & Woods, N. F. (2018). Constipation and diarrhea during the menopause transition and early postmenopause. Menopause, 25(6), 615–624. doi:10.1097/gme.0000000000001057
Castellani, D., Saldutto, P., Galica, V., Pace, G., Biferi, D., Paradiso Galatioto, G., & Vicentini, C. (2015). Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence. Urologia Internationalis, 95(4), 417–421. doi:10.1159/000381989
Maltais ML, Desroches J, Dionne IJ. Changes in muscle mass and strength after menopause. J Musculoskelet Neuronal Interact. 2009;9(4):186-97
Minkin, M. J., Reiter, S., & Maamari, R. (2015). Prevalence of postmenopausal symptoms in North America and Europe. Menopause, 22(11), 1231–1238. doi:10.1097/gme.0000000000000464
Mehta, R. S., & Staller, K. (2018). Menopausal transition and bowel disturbances. Menopause, 25(6), 589–590. doi:10.1097/gme.0000000000001110
Lanzafame, R. J., de la Torre, S., & Leibaschoff, G. H. (2019). The Rationale for Photobiomodulation Therapy of Vaginal Tissue for Treatment of Genitourinary Syndrome of Menopause: An Analysis of Its Mechanism of Action, and Current Clinical Outcomes. Photobiomodulation, photomedicine, and laser surgery, 37(7), 395–407. doi:10.1089/photob.2019.4618
**This information is for educational purposes only and is not intended to replace the advice of your doctor.

