More On How to Help Lipedema and Lymphedema
In our previous article, we went over the definitions of Lipedema and Lymphedema and just barely scratched the surface on treatment options. This article will go into more details on the different treatment options we offer at Femina Physical Therapy to help support our patients with these diagnoses.
Here are some treatments that are beneficial for both conditions.
Complete Decongestive Therapy:
CDT has 4 main components. Compression therapy, exercise, skin care, and manual lymphatic drainage.
Compression therapy:
In the case of lipedema, very light compression can help with managing pain. Light compression like yoga pants, or thigh-high compression garments with a high-rise biker short can help support the painful fat in lipedema. These garments also help support the tissues limiting the progression of fibrosis, reduce pain, and help the body move fluid out of the affected areas. For some women, their skin can be too sensitive for compression garments.
With lymphedema, compression therapy has two phases; an intensive phase, and maintenance phase. The intensive phase involves short-stretch compression bandages applied every 1-2 days by a certified lymphedema therapist (CLT) to reduce swelling (our offices have DPTs that are also CLTs). In the maintenance phase, compression garments are worn to prevent the area from reswelling. Compression therapy is tailored to individual needs and varies by the number of treatments, the way bandages are applied, and the wide range of compression garments that can be used.
Exercise:
Exercise is important in the management of lipedema, and lymphedema. Exercise combined with compression garments is best eliminating swelling, and preventing it from returning. When lymphedema is present, exercising without compression brings the risk of making swelling worse. In addition to all the other benefits of exercise, strong muscles support our circulation, and overall health and wellness. Exercise programs are individual and, in some cases, even gentle movement can help reduce swelling.
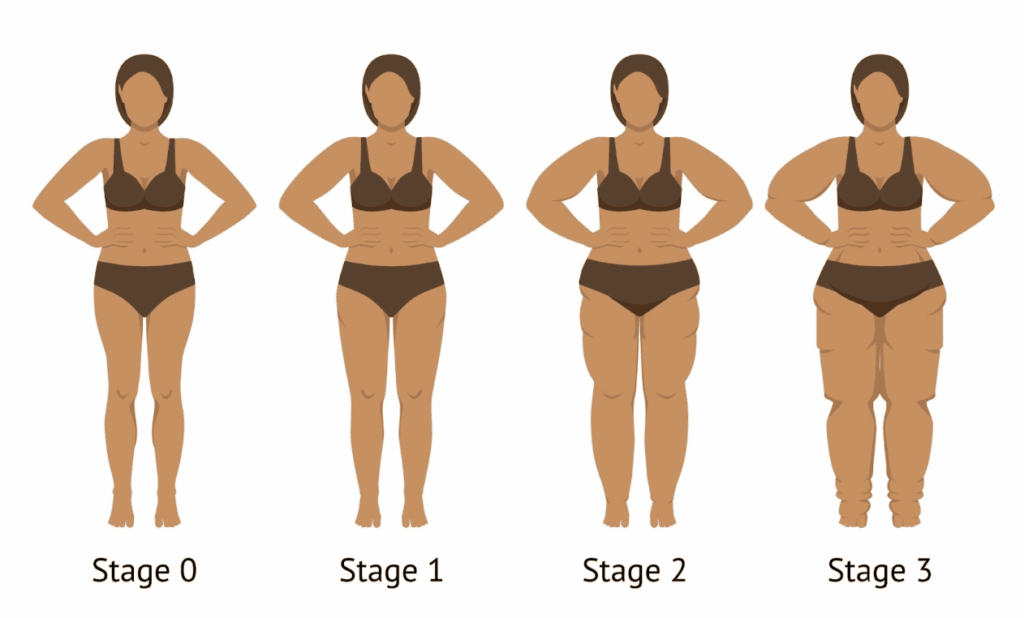
With lipedema, exercise is important independent of weight loss. Exercise helps improve circulation, metabolic function, and will help improve lymphatic flow to reduce the risk of it progressing to lipo-lymphedema (a condition when lipedema progresses, resulting in increases in pain and bruising, nodule formation under the skin, and fluid build up in the tissues that adds lymphedema to the diagnosis).
Skin care:
Since lymphedema increases risk of infection, it’s important in managing any possible bacterial or fungal infections of the skin. The skin can become dry and slow healing when swelling is present. Infections can become life threatening in the case of cellulitis, and requires medical attention.
Manual lymphatic drainage (MLD):
Manual lymphatic drainage works by manually stimulating the lymphatic system to process fluid more quickly, and to manually move/redirect fluid through the body. This technique is only skin deep and involves rhythmically stretching the skin in a specific sequence along the paths of the lymphatic system.
Light touch is needed for manual lymphatic drainage to be effective. The lymphatic system exists primarily in the skin, and deep pressure will actually close off the lymphatics, making treatment less effective. The light pressure needed for manual lymphatic drainage makes this a comfortable therapy in support of lipedema or other chronic pain conditions without provoking additional pain.
When treating lymphedema, manual lymphatic drainage is an important intervention that can help reduce mild swelling, or done right before the application of compression bandages for greater swelling reduction. It can also be used in areas of the body where greater compression is difficult to use, such as the breasts or abdomen. People with swelling can be taught self-manual lymphatic drainage, which can be beneficial in the long-term management of lymphedema.
Manual lymphatic drainage also has benefits beyond lipedema or lymphedema. It also promotes a parasympathetic nervous system response creating a relaxing effect that can also reduce pain. As a result, many people find manual lymphatic drainage to be incredibly soothing and relaxing, sometimes falling asleep during treatment. The pain and swelling reductions from manual lymphatic drainage also benefit other conditions such as abdominal bloating, chronic venous insufficiency, chronic regional pain syndrome, musculoskeletal injuries, post-operative swelling, post-traumatic swelling, fibromyalgia, rheumatoid arthritis, sinus congestion, and migraines.
There are contraindications to complete decongestive therapy and manual lymphatic drainage, so it’s best to see a physical therapist or certified lymphedema therapist for an evaluation and guidance on safe and effective treatments.
Diet:
Diet is not considered part of complete decongestive therapy, but it is important for management of overall health when living with lipedema or lymphedema. Unfortunately, there is no specific diet for the management of lymphedema, however a healthy diet is still important. Adequate protein consumption is important for balancing fluid between our veins and our body’s tissues. If serum levels of protein are too low, fluid is more likely to stay in areas affected by lymphedema.
In both cases of lymphedema and lipedema, a healthy diet can support your overall health which in turn will help you manage these conditions. Weight management is important when living with lipedema. Details of weight management are beyond the scope of this article, if you have lipedema consult with a registered dietician or physician experienced in managing lipedema before making significant changes to your diet.
You can find additional information on Lymphedema and Lipedema, or Visit Us in one of our Los Angeles offices.
References:
Joachim, E. and Steve, N. (2017) Lymphedema Management: The Comprehensive Guide for Practitioners. 4th Edition, Thieme, New York.
Vairo GL, Miller SJ, McBrier NM, Buckley WE. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based practice approach. J Man Manip Ther. 2009;17(3):e80-9. doi: 10.1179/jmt.2009.17.3.80E. PMID: 20046617; PMCID: PMC2755111.
Doubblestein, David & Sublet, Sandy & Huang, Min Hui. (2020). Effects of Manual Lymphatic Drainage Techniques on Conditions Affecting the Musculoskeletal System: A Systematic Review. 32. 92-101.
Provencher, Anne-Marie & Giguère-Lemieux, Elizabeth & Croteau, Emilie & Ruchat, Stephanie-May & Corbin-Berrigan, Laurie-Ann. (2021). The use of manual lymphatic drainage on clinical presentation of musculoskeletal injuries: A systematic review. Complementary therapies in clinical practice. 45. 10.1016/j.ctcp.2021.101469.
Schingale, Franz-Josef & Esmer, Murat & Küpeli, Buse & Ünal, Damla. (2021). Investigation of the Less Known Effects of Manual Lymphatic Drainage: A Narrative Review. Lymphatic Research and Biology. 20. 10.1089/lrb.2019.0091.
Kruppa P, Georgiou I, Biermann N, Prantl L, Klein-Weigel P, Ghods M. Lipedema-Pathogenesis, Diagnosis, and Treatment Options. Dtsch Arztebl Int. 2020 Jun 1;117(22-23):396-403. doi: 10.3238/arztebl.2020.0396. PMID: 32762835; PMCID: PMC7465366.