Learn How To Help Lipedema
This article covers the differences between Lipedema and Lymphedema and what treatment looks like for them.
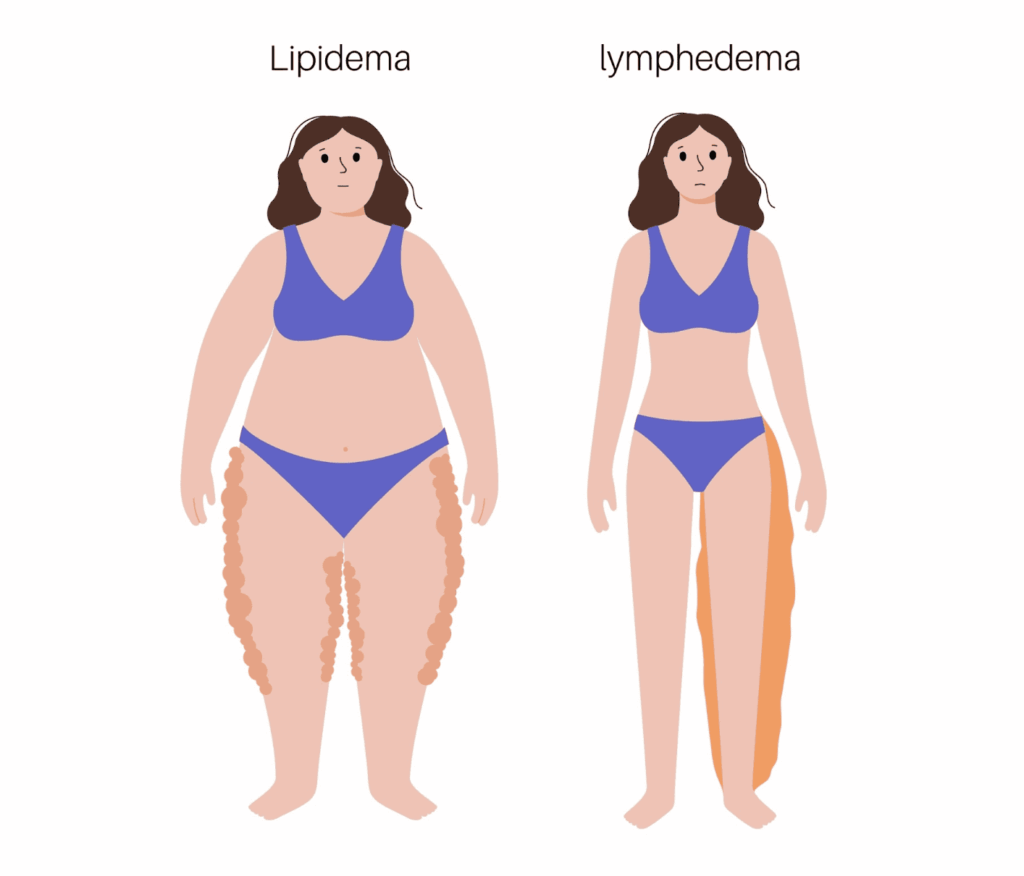
Few conditions are as prevalent and underdiagnosed as lipedema. Lipedema is the symmetrical buildup of painful subcutaneous adipose tissue (fat) and fluid in the limbs. Adipose tissue accumulates primarily in the thighs, buttocks, legs, and arms, typically without involvement in the face, hands, and feet. Lipedema is a chronic progressive condition that is frequently confused with obesity, even by healthcare providers. With obesity, adipose tissue accumulates in the entire body. Lipedema can also be present in the absence of obesity. Since lipedema is often confused with obesity, the exact prevalence is unknown. The most commonly cited prevalence in cisgender women is estimated at 11%.
Lipedema primarily affects people assigned female at birth with high levels of estrogen, and low testosterone. Lipedema has been identified in children and young adults, and some people assigned male at birth. Most people with lipedema are not diagnosed until the disease progresses to later stages and becomes difficult to manage.
The condition often goes unrecognized and people are told to lose weight. This misinformed advice as lipedema is resistant to calorie restriction. The body processes the fat in other areas of the body and lipedema remains in the thighs, hips, and upper arms. This can be dangerous advice as people may diet to the point of malnutrition without benefiting their lipedema. They might also lose muscle which is important in managing symptoms.
What are the common signs and symptoms of Lipedema?
One of the most common symptoms of lipedema is pain. The areas of the body can become very sensitive to light pressure. Easy bruising is also common, and it may not be clear what caused the bruise. Another sign of lipedema is the distribution of subcutaneous fat, primarily in the legs and buttocks and typically excludes the trunk, abdomen, hands and feet. The stemmer sign, a test for edema, is typically negative in people in the early stages of lipedema. As the condition progresses, pain and bruising increases, nodules can form under the skin, and fluid can build up in the tissues slowly progressing to lymphedema. When this happens, the condition is called lipo-lymphedema.
What is the lymphatic system?
The lymphatic system is part of our circulation and plays a role in our immune function. It’s made of tiny vessels and lymph nodes embedded in our skin and deeper tissues. These lymph nodes are clustered in the armpits, groin, abdomen, and neck.
One of the key roles of the lymphatic system is to transport lymph; a thick fluid rich in protein, cellular components, cells, anything that is too large to re enter our veins.
What is lymphedema and what causes it?
Lymphedema is the buildup of lymph in tissues, caused by impairment of the lymphatic system. Lymphedema occurs most commonly in the arms or legs, but can also occur in the head and neck, the breasts, abdomen, and genitals. Involvement of the limbs is usually asymmetrical; for example, even when both legs are involved, one is usually worse than the other.
Lymphedema can be divided into primary and secondary lymphedema. Primary lymphedema is hereditary or congenital and swelling is often diagnosed in early life. Secondary lymphedema is caused by damage to the lymphatic system. In the United States, the most common causes of secondary lymphedema are treatments (surgical and radiation) for breast cancer, chronic venous insufficiency, and treatments for other cancers. There is no cure for lymphedema, but treatments are effective for managing the condition.
Treatment is important as lymphedema impairs the immune system in the affected area and can significantly increase the risk of infection. Bacterial infections can progress to cellulitis which requires immediate medical attention. Cellulitis typically appears as a rash, very painful to the touch, often accompanied by a fever, and can progress quickly. Cellulitis can be life threatening and should be treated immediately. It may appear as a streak on the affected limb that moves closer to the person’s center.
What are the common symptoms of lymphedema?
The symptoms of lymphedema change as the condition progresses. Swelling appears in stage 1 lymphedema. The swelling is soft and reversible when elevating the affected area. In stage 2 swelling is no longer reversible and the edema starts to become firm. The skin can also begin to change and become fibrotic and hard. Skin infections and slow healing become more common, and the stemmer sign is positive. In stage 3 lymphedema, skin texture changes significantly and the affected body part can become significantly larger.
How are these conditions treated?
Treatments for lipedema and lymphedema are similar. Complete decongestive therapy (CDT) can be a key therapy in reducing swelling, managing pain, and slow/limit the progression of Lipedema and Lymphedema. In the case of lipedema, liposuction can be an effective way to reduce the accumulation of subcutaneous adipose tissue. The full scope of treatments for lipedema is beyond the scope of this article, and more information can be found at the Lipedema Foundation.
In Part 2 we dive further into the treatments for Lipedema and Lymphedema at Femina Physical Therapy. You can find additional information on Lymphedema and Lipedema, or Visit Us in one of our Los Angeles offices for treatment.
References:
Joachim, E. and Steve, N. (2017) Lymphedema Management: The Comprehensive Guide for Practitioners. 4th Edition, Thieme, New York.
Vairo GL, Miller SJ, McBrier NM, Buckley WE. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based practice approach. J Man Manip Ther. 2009;17(3):e80-9. doi: 10.1179/jmt.2009.17.3.80E. PMID: 20046617; PMCID: PMC2755111.
Doubblestein, David & Sublet, Sandy & Huang, Min Hui. (2020). Effects of Manual Lymphatic Drainage Techniques on Conditions Affecting the Musculoskeletal System: A Systematic Review. 32. 92-101.
Provencher, Anne-Marie & Giguère-Lemieux, Elizabeth & Croteau, Emilie & Ruchat, Stephanie-May & Corbin-Berrigan, Laurie-Ann. (2021). The use of manual lymphatic drainage on clinical presentation of musculoskeletal injuries: A systematic review. Complementary therapies in clinical practice. 45. 10.1016/j.ctcp.2021.101469.
Schingale, Franz-Josef & Esmer, Murat & Küpeli, Buse & Ünal, Damla. (2021). Investigation of the Less Known Effects of Manual Lymphatic Drainage: A Narrative Review. Lymphatic Research and Biology. 20. 10.1089/lrb.2019.0091.
Kruppa P, Georgiou I, Biermann N, Prantl L, Klein-Weigel P, Ghods M. Lipedema-Pathogenesis, Diagnosis, and Treatment Options. Dtsch Arztebl Int. 2020 Jun 1;117(22-23):396-403. doi: 10.3238/arztebl.2020.0396. PMID: 32762835; PMCID: PMC7465366.