We Take a Look at Combined Methods of Hormonal Birth Control and Vulvodynia
In this three part series, we will explore the effects of hormonal contraceptive methods and their relationship with vulvodynia.
What is Hormonal Birth Control?
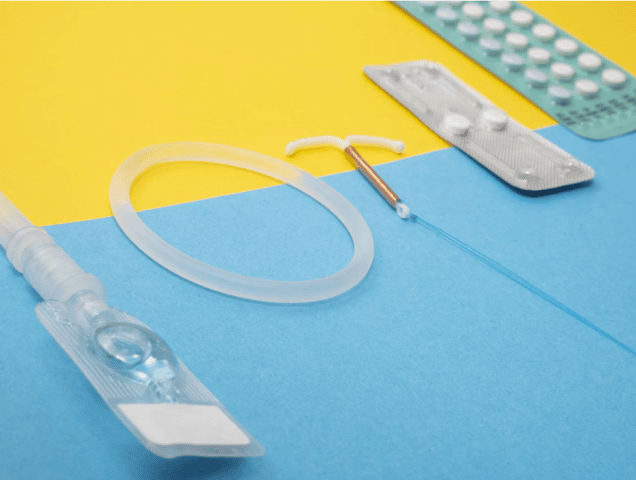
Hormonal birth control methods, such as birth control pills, patches, injections, rings and hormonal intrauterine devices (IUDs), work by altering hormone levels in the body to prevent pregnancy. Hormonal contraceptives fall into two categories: combined, meaning they contain both estrogen and progestin (think the pill, patch, or ring), or contain progestin only (think progestin only pill or “POP”, arm implant, IUDs, or injections). While the primary intent of these drugs are for contraception, they are also widely prescribed for other common issues such as: mood imbalance related to periods, skin issues, irregular periods, and painful periods.
What effect could Hormonal Birth Control have on my body?
While these methods are highly effective for contraception, they can also influence hormonal balance and exacerbate symptoms for individuals with vulvodynia or create an onset of vulvodynia for some individuals. Vulvodynia is pain on the vulva, or external genital tissue. For more information about vulvodynia, check out this post on our website.
It has now been well established that there is a relationship between onset of vulvodynia and initiation of combined hormonal birth control pills1,2,3,4,5. However, what about other options, such as the vaginal ring, patch or IUD?
First, let’s explore combined hormonal contraceptive methods and the onset of vulvodynia:
Combined hormonal birth control methods impact the tissues of the vagina and the vulva by decreasing the amount of circulating sex hormones–estrogen and androgens– leading to decreased pelvic blood flow, increased vaginal and vestibular (the opening to the vagina) atrophy, and decreased lubrication1. Most research on vulvodynia and hormonal birth control have been conducted using combined oral contraceptive pills. The following research findings are all specific to the combination pill:
- When comparing controls of women who are not on the pill, women on combined hormonal contraceptives had thinner skin at the opening of the vagina, making this tissue more vulnerable to mechanical strain1 (Think, the tissue may tear)
- Another study also found decreased pain thresholds at the opening of the vagina, or vestibule, of women taking the pill compared to controls who were not on birth control2
- Several studies have also found women who started the pill at a young age were 11 and 10 times more likely to develop vulvodynia later in life compared to women who had never taken the pill3
- However, when the pill is given with higher levels of estrogen, and in an extended cycle, women have shown a decrease in pain with sex5
What about the patch or the ring?
The patch and the ring can also decrease the amount of overall circulating sex hormones and can lead to the same previously discussed vaginal side effects. Studies have even shown the patch or ring can decrease the amount of circulating sex hormones even more than the pill does4,5. However, a recent preliminary study of women without pelvic floor or sexual dysfunction found an increase in sexual function in women using an extended nuvaring (64 days with ring in, 4 days with ring out) across the following categories: desire, lubrication, orgasm, pain with sex4. Another study found one participant developed vaginal dysbiosis after starting the ring, who had a prior history of recurrent vaginal infections and vestibulodynia.The study concluded with a caution about prescription of vaginal rings in patients with a history of recurrent vaginal infections and/or vulvodynia7.
A recent randomized trial looked at sexual function in new ring (not extended use as the prior mentioned study) and patch users who had recently switched from using the pill. Interestingly, ring users had a decrease in overall sexual function, one of the significant categories being pain, while patch users had an increase in sexual function6. Currently, not enough research has been published either way to be conclusive about the relationship between nuvaring or patch and vulvodynia. However, it may be beneficial to discuss with your physician if you are experiencing new onset of symptoms of vulvodynia while on a vaginal or patch delivered combined hormonal contraceptive to explore other options of birth control.
Managing Hormonal Birth Control and Vulvodynia
Vulvodynia is a multifactorial condition, with many contributing causes including: physiological, sexual, psychological and interpersonal. While hormonal birth control can either aggravate or create an onset of vulvar pain, it cannot be blamed as the only cause, and more research is being conducted to explore this relationship continually, as there may be a genetic predisposition that explains why some women will develop vulvodynia on hormonal birth control while others may not1.
Navigating the intersection of hormonal birth control and vulvodynia requires a personalized approach tailored to individual needs and preferences. Here are some strategies to consider:
- Consultation with Healthcare Providers: Individuals with vulvodynia considering hormonal birth control should consult with healthcare providers specializing in vulvar conditions or sexual medicine.
- In addition to contraceptive considerations, managing vulvodynia often requires a holistic approach that addresses various factors contributing to symptoms. This may include pelvic floor physical therapy, pain management techniques, lifestyle modifications, and psychological support.
At Femina Physical Therapy, all of our physical therapists have specialized training to address the musculoskeletal components of your pain and will work with your other healthcare providers in a collaborative manner to maximize symptom-relief and improve your quality of life. Reach out to our team to get started.
Interested to learn more? Click here to read Part 2 and Part 3.
Resources:
- Aerts L.,Pluchino N., Hormonal contraception and vulvodynia: an update, GREM Gynecological and Reproductive Endocrinology & Metabolism (2021); 03/2021:156-161 doi: 10.53260/GREM.212034
- Bohm-Starke N, Johannesson U, Hilliges M, Rylander E, Torebjörk E. Decreased mechanical pain threshold in the vestibular mucosa of women using oral contraceptives: a contributing factor in vulvar vestibulitis?. J Reprod Med. 2004;49(11):888-892.
- Bouchard C, Brisson J, Fortier M, Morin C, Blanchette C. Use of oral contraceptive pills and vulvar vestibulitis: a case-control study. Am J Epidemiol. 2002;156(3):254-261. doi:10.1093/aje/kwf037
- Burrows LJ, Basha M, Goldstein AT. The effects of hormonal contraceptives on female sexuality: a review. J Sex Med. 2012;9(9):2213-2223. doi:10.1111/j.1743-6109.2012.02848.x
- de Castro Coelho F, Barros C. The Potential of Hormonal Contraception to Influence Female Sexuality. Int J Reprod Med. 2019;2019:9701384. Published 2019 Mar 3. doi:10.1155/2019/9701384
- Gracia CR, Sammel MD, Charlesworth S, Lin H, Barnhart KT, Creinin MD. Sexual function in first-time contraceptive ring and contraceptive patch users. Fertil Steril. 2010;93(1):21-28. doi:10.1016/j.fertnstert.2008.09.066
- Murina F, Graziottin A, Di Francesco S, Recalcati D. The impact of combined contraceptive vaginal ring on vaginal environment: an observational, longitudinal study. Eur J Contracept Reprod Health Care. 2023;28(4):234-237. doi:10.1080/13625187.2023.2228440
- https://www.acog.org/womens-health/faqs/combined-hormonal-birth-control-pill-patch-ring#:~:text=Birth%20control%20pills%2C%20the%20birth,progestin%20into%20the%20whole%20body.
More Articles in This Series
{modulepos position=”birthcontrol”}