During pregnancy, the body goes through tremendous changes that can significantly impact strength, endurance, and ability to absorb ground reaction forces that are required to safely return to running. Your growing belly changes your posture, your hormones are making your joints more flexible, and some amount of deconditioning is expected and normal as pregnancy progresses.
For most postpartum runners, their return to running following birth can be intimidating and overwhelming.
A woman's OBGYN will commonly clear her for exercise at six weeks postpartum if she is not bleeding. According to guidelines published by Tom Goom and others, most women aren't ready to return to running or impact for twelve weeks postpartum due to significant healing needs. As with most things, healing takes time, and some women may need to wait even longer to return to running. Breastfeeding mothers, women experiencing fatigue, sleep deprivation, or inadequate nutrition may need additional before getting back to running. Nevertheless, this does not mean you should be sedentary for your baby's first 3 months! To prepare your body for impact, you can focus on low impact exercises and activities in the meantime:
Walk before you run -
Start with increasing your steps gradually. Start with a 10 minute walk daily, increasing by 5 minutes each week to add some light cardiovascular activity into your routine, with the goal of being able to walk for 30 minutes without fatigue, pain or pelvic floor related symptoms.
Focus on your breath -
During postpartum, breath work can help you breathe more efficiently and help you recover faster. Focus on diaphragmatic breathing. Allow your belly to fill on the inhale, and relax and soften on the exhale.
Prioritize core and pelvic floor bracing -
After you’ve mastered your breathwork, start to add gentle core bracing and pelvic floor contractions. If you are not sure how to activate your core or pelvic floor, it’s best to speak to a pelvic floor physical therapist to ensure that you are performing this properly.
Check out this previous blog post we wrote for some exercise inspiration.
Are you at least 3 months postpartum and unsure if your body is ready to return to running? Try this simple self test!
First, assess the health and function of your pelvic floor muscles. Ask yourself the following questions:
- Do you experience urine, stool or gas leakage when you cough/sneeze/laugh/ exercise?
- Do you have a bulge or sense something falling out of the vaginal area?
- Do you experience pain with bowel movements, tampon use, or intercourse?
- Can you walk 30 minutes or longer without onset of symptoms?
If your answer is ‘yes’ to any of these above questions, then it is recommended to have your pelvic floor evaluated by a pelvic health physical therapist. You can make an appointment to see one of us here.
However, if your answer is ‘no’, then you may be ready to be screened for your readiness to run. (yes, we do that, too!) Everyone needs good baseline strength and coordination of the lower extremities in order to run.
Try the following return to running assessment:
- Single leg calf raise, 20 repetitions
- Single leg sit to stand, 20 repetitions
- Single leg bridge, 20 repetitions
- Side-lying hip abduction, 20 repetitions
- Single leg running man, 20 repetitions
- 30 second single leg stance
- Jogging on the spot for 1 minute
- Single leg hopping in place
If these drills feel good, then you may be ready to trial some running! Experts on postpartum rehabilitation recommend following a run/walk protocol, slowly increasing the time that you are running each week. Here is a simple example: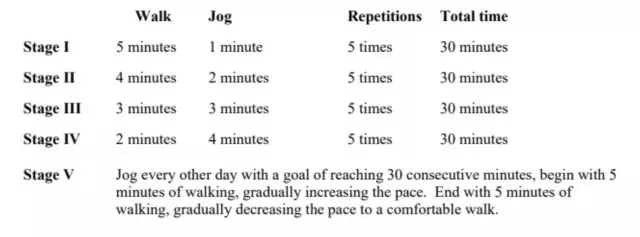
If you do experience any vaginal heaviness, urinary leakage or pain with the above exercises, then it is strongly advised to get your pelvic floor examined by a physical therapist prior to returning to running or other forms of high impact exercise.
Still have questions? At Fusion Wellness & Femina Physical Therapy, our team of expert physical therapists can assess your pelvic floor and whole body to determine your readiness to return to these activities and reduce your risk of injury.
References:
- Goom T, Donnelly E, Brockwell E. Returning to running postnatal—guidelines for medical, health and fitness professionals managing this population. https:// www.absolute.physio/wp-content/uploads/2019/09/returning-to-runningpostnatal-guidelines.pdf. Published 2019. Accessed May 28, 2021
- Christopher, Shefali & Gallagher, Sandra & Olson, Amanda & Cichowski, Sara & Deering, Rita. (2022). Rehabilitation of the Postpartum Runner: A 4-Phase Approach. Journal of Women's Health Physical Therapy. Publish Ahead of Print. 10.1097/JWH.0000000000000230.













